More Information
Submitted: May 21, 2022 | Approved: August 26, 2022 | Published: August 29, 2022
How to cite this article: Rodríguez-García M, Silva-Peña L, Aparicio-García C, Lewandrowski KU. Cervical disc arthroplasty, challenges and indications: case report. Arch Clin Exp Orthop. 2022; 6: 001-004.
DOI: 10.29328/journal.aceo.1001010
Copyright Licence: © 2022 Rodríguez-García M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cervical disc arthroplasty, challenges and indications: case report
Manuel Rodríguez-García1* , Liliana Silva-Peña1, Carlos Aparicio-García1 and Kai-Uwe Lewandrowski2
, Liliana Silva-Peña1, Carlos Aparicio-García1 and Kai-Uwe Lewandrowski2
1The American British Cowdray Medical Center, Santa Fe I.A.P Neurology, Orthopedics and Rehabilitation Center, México
2Center For Advanced Spine Care of Southern Arizona and Surgical Institute of Tucson, Tucson AZ, USA
*Address for Correspondence: Manuel Rodríguez-García, The American British Cowdray Medical Center, Santa Fe I.A.P Neurology, Orthopedics and Rehabilitation Center, México, Email: [email protected]
Degenerative changes in the intervertebral discs can cause a significant impact on the biomechanics of the spine this can result in compression of the nerve roots or the spinal cord [1].
In previous years, Anterior Cervical Discectomy and Fusion (ACDF) became the gold standard for the treatment of symptomatic cervical disease [2]. This procedure results in loss of mobility in the intervened segment and this conditioning an increase in tension in the adjacent segments, thus contributing to the adjacent segment syndrome [3]. The disadvantages of this technique include limitation or loss of cervical mobility, increased intradiscal pressure and pseudoarthrosis.
Currently, cervical disc arthroplasty is considered an acceptable surgical treatment for cervical radiculopathy and myelopathy, developed to preserve the subaxial biomechanics of the cervical spine. In the United States, total cervical spinal arthroplasty is approved by the Federal Drug Administration (FDA) for use at 1 and 2 levels for cervical disc disease resulting in myelopathy and/or radiculopathy between C3 - C7 [4].
The indications for a cervical disc arthroplasty are young, active adult patients with disc disease that causes symptoms at one and up to two levels from C3 to C7 without alteration in the facet joints or instability. Absolute contraindications are a significant decrease in the intervertebral space with loss of mobility at that level, osteoarthritis of the zygapophyseal joint, significant deformity in the sagittal and coronal planes, segmental instability, local or systemic infection [5,6].
A 38-year-old male. Pathological personal history: pyloroplasty at birth, lumbar instrumentation L4 - L5 and L5-S1 in 2008 (14 years ago), right Achilles tendon plasty in 2018. Allergies were denied.
His clinical condition began with cervical and interscapular pain radiating to the lateral region of both arms but was more intense in the right arm and forearm with altered sensitivity of the second and third fingers of the right hand that increased with prolonged positions, which partially improved with neuromodulatory treatment.
On physical examination, the pain increased on extension, flexion, and lateral flexion of the neck, kyphotic posture, Spurling absent and pain on palpation of bilateral paravertebral muscles, predominantly lower cervical. Right thumb extension weakness at +4/5. Muscle stretch reflexes Biceps bilateral with the normal response and hyporeflexia at the right triceps. Sensitivity with hypoalgesia external face of the right arm.
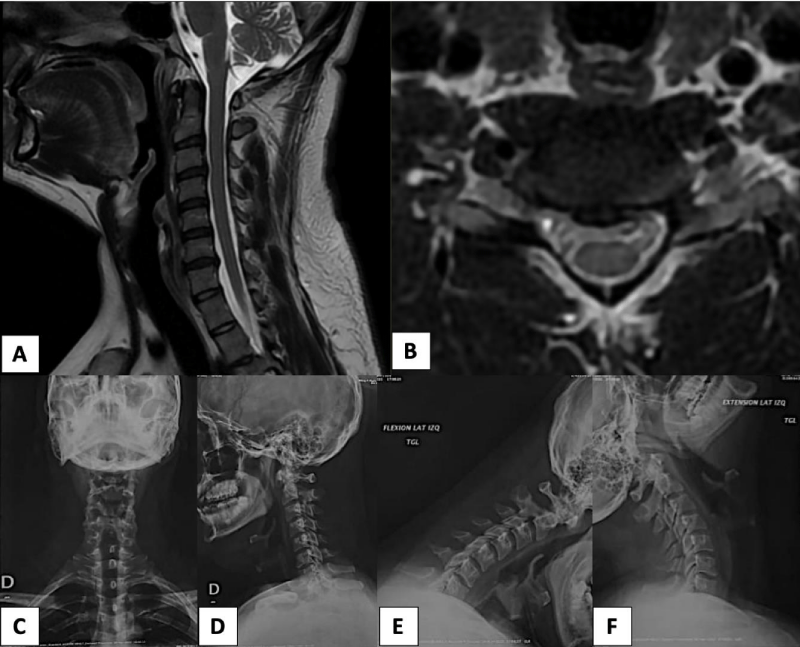
Magnetic Resonance showed decreased C6 - C7 inter somatic space, right foraminal disc protrusion C6 - C7, and degenerative disc disease C6 - C7 is observed. X-rays of the cervical spine are performed with anteroposterior, lateral and dynamic views to rule out the presence of instability (listhesis) which would contraindicate the use of cervical prosthetics, The patient radiographs showed decreased inter somatic space C6 - C7 without instability and rectification of cervical lordosis due to muscular contracture (Image 1).
Diagnosis of C6 - C7 foraminal disc herniation is integrated. It is scheduled for surgical treatment which is performed on May 06, 2022, for Total Cervical Arthroplasty C6 - C7.
Surgical technique
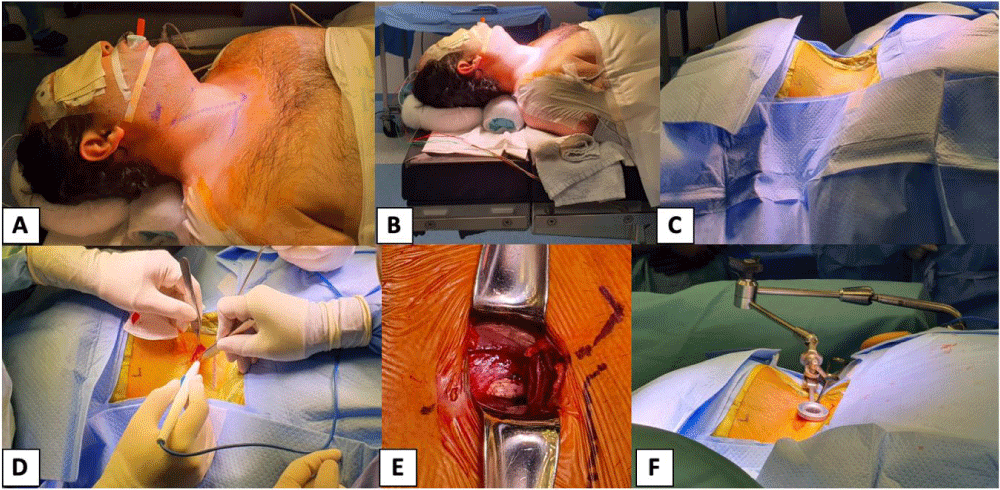
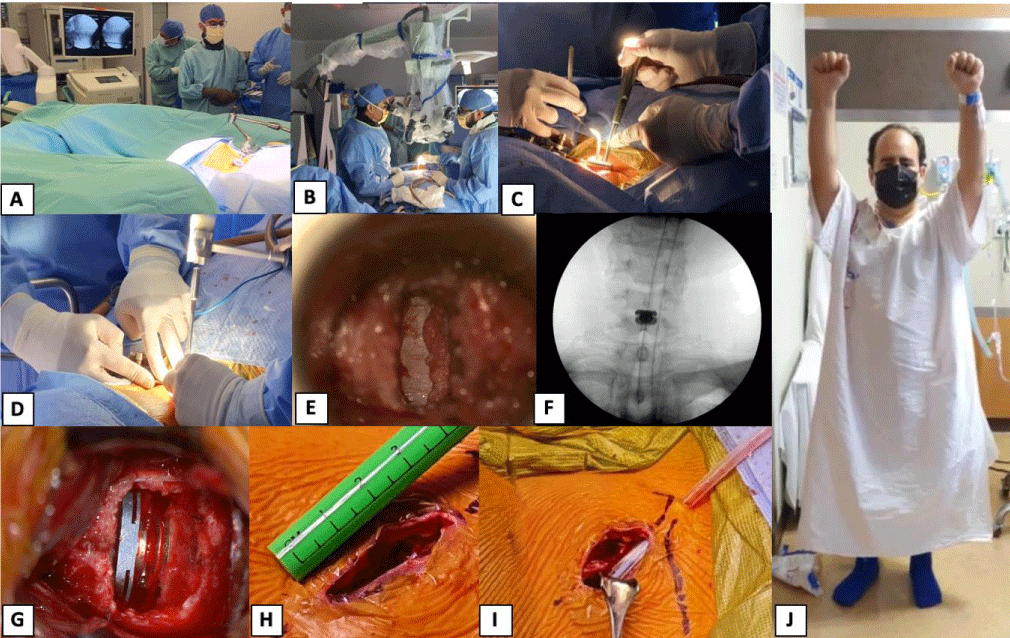
1. Under general intravenous anesthesia and neurophysiological monitoring, 2. The patient is placed in the supine position, 3. Asepsis and antisepsis of the cervical region and placement of sterile fields, 4. Radiological marking like Smith Robinson is performed (anterolateral), 5. Longitudinal incision of 3 cm and dissection by planes, 6. Tubular retractor is placed under fluoroscopic vision locating level C6 - C7 (Image 2), 7. Discectomy is performed under microscope magnification, 8. Plate curettage terminals, 9. The dural sac is exposed 10. Placement of ROTAIO 15 × 13 × 7 mm prosthesis under fluoroscopic control confirming its adequate placement, 11. Review of hemostasis, 12. Placement of drainage on the contrary opening, 13. Closure by planes (Image 3).
Image 1: Preoperative Magnetic Resonance Imaging (MRI). A and B) preoperative cervical MRI. A) Cervical MR in the sagittal view at the level of C6-C7 notes the left bilateral foraminal stenosis with a predominance of the left foramen. C, D, E, F) at the level of C6-C7 decreased inter somatic space without instability.
Image 2: Transoperative Images. A) Surgical marking for anterolateral approach (Smith Robinson). B) Cranium and interscapular wedge are placed and shoulder traction with the intention of avoiding the interposition of the shoulders with the neck during fluoroscopy. D) Dissection by planes with previous asepsis, antisepsis, and sterile fields are placed. E) exposure of the paravertebral muscles and the intervertebral space. F) Placement of the tubular retraction system.
Image 3: Transoperative Images. A) Proper placement of the tubular retraction system is confirmed by fluoroscopy. B) The surgical microscope is positioned to start the microsurgical discectomy. C, D) The procedure is performed completely through the tubular retractor by the main surgeon with an assistant. E) Complete discectomy with exposure of the dural sac, confirming adequate decompression of the canal. F, G) The correct placement of the cervical prosthesis (ROTAIO) is confirmed by fluoroscopy and under the surgical microscope. H, I) The procedure ends with an incision of approximately 3 cm long, a Jackson Pratt drain is placed next to the skin incision, and closure is performed by layers. J) Immediate postoperative. The patient presents a clinical improvement in muscle strength and total absence of preoperative pain.
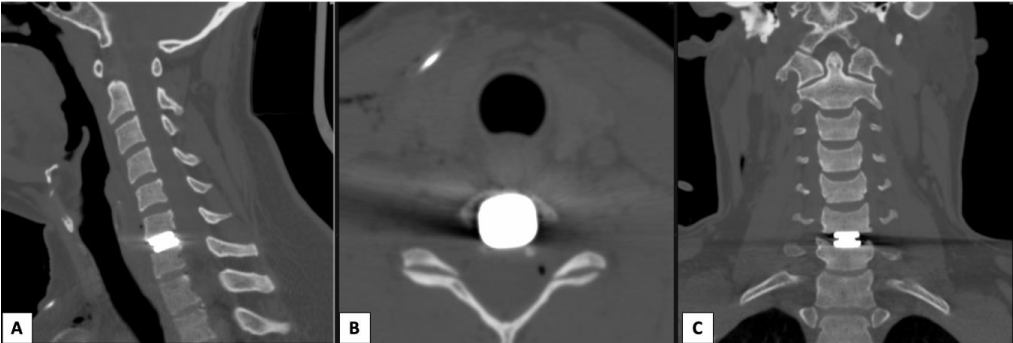
The patient reported clinical improvement after surgery, upper extremities with strength 5/5 and sensitivity 2/2. Simple postoperative tomography of the cervical spine is performed, observing the proper placement of the implant (Image 4). He is discharged home 2 days after surgery to continue with physical therapy and rehabilitation and follow-up by outpatient consultation. A cervical collar was indicated for two weeks long until good recovery of the surgical wound showed good recovery.
Image 4: Immediate postoperative Computed Tomography (CT). A,C,D) CT at the sagittal, axial and coronal views, the correct position of the cervical prosthesis is confirmed. B) In the axial cut bilateral foraminal decompression is noted.
It is established that surgical cervical decompression is an effective treatment option for cervical spondylitis that stops the progression of symptoms while promoting signi-ficant functional recovery [7,8]. Surgical decompression can be performed through an anterior or a posterior surgical approach. Subsequent surgery usually involves a laminoplasty or laminectomy with fusion [9].
The decision of the approach depends on the cause of the neurological compression (anterior or posterior, or both), the number of segments involved, and the experience of the surgeon’s approach [10,11]. In anterior decompression, the existence of herniated discs or hypertrophy of the uncovertebral joint is clearly observed and, therefore, it is possible to perform a direct root decompression. Laminoplasty will not improve root decompression due to foraminal stenosis, however, a laminotomy with cervical foraminotomy is capable of relieving symptoms of the spinal cord and root compression [12].
In 2017, Laratta, et al. conducted a systematic review of comprehensive review of single-level cervical disc arthroplasty, multilevel and hybrid procedures, in which they report that, over the last decade, multiple high-quality studies have reported that single-level cervical disc arthroplasty offers equivalent clinical results with a reduction of secondary procedures when compared to patients undergoing ACDF [2], however, in recent studies the prevalence is increasing in 2-level cervical disc arthroplasty and hybrid surgery, the second seems to be as effective as its single-level counterparts, however, it requires more studies [13].
A study by Fay, et al. 2014, demonstrates the differences between anterior cervical arthroplasty and fusion in bilevel cervical degenerative disc disease, as a result, cervical arthroplasty preserved mobility in the operating segments and provided clinical results similar to those of ACDF at 39.6 months of follow-up [14].
Regarding the precautions and recommendations of the anterolateral approach for cervical disc arthroplasty, the following have been described:
The position of the neck in slight hyperextension without excessive traction, the combination of hyperextension and excessive traction of the head can condition compression of the tissues, the laryngeal nerves may be at risk of injury as a result of such positioning [15]. Rigid support of the neck is essential to prevent complications when force is applied to the vertebral body. Also, excessive shoulder pull can cause brachial plexus injury.
The anterolateral cervical approach is generally safe, however, the complications that have been reported and how to avoid them must be taken into account, these include vascular, neurological, soft tissue, and visceral complications [16].
It is important to widely know the indications and contraindications to perform this procedure and thus avoid complications. As for the anterolateral cervical approach, it is performed through a relatively safe anatomical plane, however, it is important to know the anatomy and customize the approach according to the characteristics of each patient (neck morphology, level of intervention, etc.), in this case, a longitudinal anterolateral approach was perform since the patient had a wide and short neck, typical seen in short stature and obese patients.
Cervical disc arthroplasty is currently a widely accepted surgical procedure for the treatment of radiculopathy and/or cervical myelopathy. Its main advantage over anterior cervical discectomy and fusion is the preservation of segment mobility, resulting in reduced stress. In the adjacent segments and thus avoiding adjacent segment disease.
- Piere P. Cervical Spine Minimally Invasive and Open Surgery. Springer. 2016.
- Laratta JL, Shillingford JN, Saifi C, Riew KD. Cervical Disc Arthroplasty: A Comprehensive Review of Single-Level, Multilevel, and Hybrid Procedures. Global Spine J. 2018 Feb;8(1):78-83. doi: 10.1177/2192568217701095. Epub 2017 May 16. PMID: 29456918; PMCID: PMC5810892.
- Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005 Dec;3(6):417-23. doi: 10.3171/spi.2005.3.6.0417. PMID: 16381202.
- Truumees E. Cervical and lumbar disk replacement. In: Rao RD, Smuck M, eds. Orthopaedic Knowledge Update: Spine, 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons. 2012; 371-393.
- Jia Z, Mo Z, Ding F, He Q, Fan Y, Ruan D. Hybrid surgery for multilevel cervical degenerative disc diseases: a systematic review of biomechanical and clinical evidence. Eur Spine J. 2014 Aug;23(8):1619-32. doi: 10.1007/s00586-014-3389-5. Epub 2014 Jun 8. PMID: 24908252.
- Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004 Sep 15;17(3):E9. doi: 10.3171/foc.2004.17.3.9. PMID: 15636565.
- Furlan JC, Kalsi-Ryan S, Kailaya-Vasan A, Massicotte EM, Fehlings MG. Functional and clinical outcomes following surgical treatment in patients with cervical spondylotic myelopathy: a prospective study of 81 cases. J Neurosurg Spine. 2011 Mar;14(3):348-55. doi: 10.3171/2010.10.SPINE091029. Epub 2011 Jan 14. PMID: 21235299.
- Sampath P, Bendebba M, Davis JD, Ducker TB. Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976). 2000 Mar 15;25(6):670-6. doi: 10.1097/00007632-200003150-00004. PMID: 10752097.
- Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000 Oct;93(2 Suppl):199-204. doi: 10.3171/spi.2000.93.2.0199. PMID: 11012049.
- Mummaneni PV, Kaiser MG, Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK; Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009 Aug;11(2):130-41. doi: 10.3171/2009.3.SPINE08728. PMID: 19769492.
- Rao RD, Currier BL, Albert TJ, Bono CM, Marawar SV, Poelstra KA, Eck JC. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am. 2007 Jun;89(6):1360-78. doi: 10.2106/00004623-200706000-00026. PMID: 17575617.
- Koshu K, Tominaga T, Yoshimoto T. Spinous process-splitting laminoplasty with an extended foraminotomy for cervical myelopathy. Neurosurgery. 1995 Sep;37(3):430-4; discussion 434-5. doi: 10.1227/00006123-199509000-00010. PMID: 7501107.
- Gandhi AA, Kode S, DeVries NA, Grosland NM, Smucker JD, Fredericks DC. Biomechanical Analysis of Cervical Disc Replacement and Fusion Using Single Level, Two Level, and Hybrid Constructs. Spine (Phila Pa 1976). 2015 Oct 15;40(20):1578-85. doi: 10.1097/BRS.0000000000001044. PMID: 26165217.
- Fay LY, Huang WC, Tsai TY, Wu JC, Ko CC, Tu TH, Wu CL, Cheng H. Differences between arthroplasty and anterior cervical fusion in two-level cervical degenerative disc disease. Eur Spine J. 2014 Mar;23(3):627-34. doi: 10.1007/s00586-013-3123-8. Epub 2013 Dec 7. PMID: 24318106; PMCID: PMC3940787.
- Denaro V. Stenosis of the cervical spine. Springer, Berlin 1991.
- Patel NP, Wolcott WP, Johnson JP, Cambron H, Lewin M, McBride D, Batzdorf U. Esophageal injury associated with anterior cervical spine surgery. Surg Neurol. 2008 Jan;69(1):20-4; discission 24. doi: 10.1016/j.surneu.2007.05.006. Epub 2007 Oct 31. PMID: 17976697.