More Information
Submitted: March 05, 2024 | Approved: March 27, 2024 | Published: March 28, 2024
How to cite this article: García AC, Mateo SG, Pérez MR, Gil JCS, Álvarez MTG, et al. Persistent Lumbar Pain and Fever: Osteomyelitis as Diagnosis Challenge. Arch Clin Exp Orthop. 2024; 8: 005-009.
DOI: 10.29328/journal.aceo.1001019
Copyright Licence: © 2024 García AC, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Osteomyelitis; Lumbar pain; Fever; Spondylodiscitis; Infectious spondylitis; Diagnostic challenges; Urological complications
Persistent Lumbar Pain and Fever: Osteomyelitis as Diagnosis Challenge
Alicia Cárdenas García1*, Sara García Mateo2, María Rodríguez Pérez2, José Carlos Sureda Gil1, María Teresa Gómez Álvarez3, Francisco de Borja Hernández Moreno3 and Anna de Paola Prato2
1Third-year Medical Resident, Villalba General Hospital, Madrid, Spain
2Second-year Medical Resident, Villalba General Hospital, Madrid, Spain
3Specialist Doctor, Villalba General Hospital, Madrid, Spain
*Address for Correspondence: Alicia Cárdenas García, Third-year Medical Resident, Villalba General Hospital, Madrid, Spain, Email: [email protected]
Objective: This study aimed to evaluate the clinical characteristics and diagnostic challenges associated with osteomyelitis in patients presenting with persistent lumbar pain and fever.
Methods: We conducted a descriptive observational study, reviewing four cases of osteomyelitis diagnosed at our hospital’s Emergency Department in 2022. Data on patient demographics, medical history, clinical presentation, diagnostic methods, and treatment outcomes were analyzed.
Findings: The cases included middle-aged to elderly men, with predisposing factors such as urological interventions and immunodeficiency. Imaging studies, particularly CT-scan and MRI, were instrumental in diagnosing lumbar spondylodiscitis. Biopsies revealed lymphoplasmacytic infiltrates and treatment responses were positive in all cases after eight months of follow-up. The study highlights the importance of considering osteomyelitis in the differential diagnosis of lumbar pain and fever, necessitating multidisciplinary collaboration for timely management.
Osteomyelitis, characterized by inflammation and infection of the bone, could be caused by local dissemination or distant hematogenous dissemination. It poses diagnostic challenges, particularly when presenting with symptoms such as lumbar pain and fever [1,2]. Among the various manifestations of osteomyelitis, spondylodiscitis, an infectious process affecting the vertebral bodies and intervertebral discs, represents a formidable clinical entity. Infectious spondylitis, encompassing conditions such as spondylodiscitis, warrants prompt recognition and management due to its potential for severe morbidity and complications.
In clinical practice, the diagnosis of osteomyelitis, especially in the context of lumbar pain and fever, often requires a comprehensive evaluation to differentiate it from other causes. The presence of urological complications further complicates the diagnostic process, as seen in cases following prostatic adenocarcinoma treatments or post-surgical interventions. The interplay between predisposing factors, such as immunodeficiency, and the clinical presentation of osteomyelitis underscores the importance of a nuanced approach to diagnosis and management.
This introduction sets the stage for exploring the diagnostic challenges inherent in identifying osteomyelitis, particularly within the context of lumbar pain, fever, and associated urological complications [1-3]. By examining the clinical characteristics and outcomes of cases presenting with these features, we aim to shed light on the complexities of diagnosing and managing infectious spondylitis, thereby improving patient care and outcomes. This study exposes four different cases that happened in our hospital in 2022.
Objective
Evaluation of patients’ clinical characteristics and similitude search between the cases diagnosed at the Emergency Department in our hospital [4,5].
Observational descriptive study
Patient information: Patient data for this observational descriptive study were collected from medical records of individuals presenting with lumbar pain and fever at the Emergency Department of [Hospital Name] during the year 2022. The study cohort comprised four patients, herein referred to as Patient 1, Patient 2, Patient 3, and Patient 4 [6-8].
Clinical staff: The patients were evaluated by a multidisciplinary team including emergency physicians, infectious disease specialists, radiologists, and orthopedic surgeons.
Total number of patients: During the study period, a total of 1480 patients visited the Emergency Department with complaints of lumbar pain and fever in one year (2022).
Data collection: Patient demographics, medical history, clinical presentation, diagnostic procedures, treatment modalities, and outcomes were extracted from electronic medical records. Imaging studies including CT-scan and MRI were reviewed for diagnostic purposes. Histopathological findings from bone biopsies were also analyzed. The information gathered was collated and analyzed to identify commonalities and variations among the cases [9-11] (Table 1).
| Table 1: Patient Characteristics. | ||||||
| Patient | Age | Gender | Past Medical History | Clinical Presentation | Diagnostic Findings | Treatment |
| Patient 1 | 69 y/o | Male | Hypertension, prostatic adenocarcinoma treated with radical prostatectomy | Lumbar pain, fever | T9-T10 spondylodiscitis, negative bone biopsies, infectious assumed | Long antibiotic therapy |
| Patient 2 | 46 y/o | Male | None | Lumbar pain, fever, chills | L3-L4 spondylodiscitis, methicillin-susceptible Staphylococcus aureus from blood cultures | Antibiotic therapy, identified immunoglobulin A deficiency |
| Patient 3 | 72 y/o | Male | Prostatic adenocarcinoma treated with transurethral resection | Lumbar pain, fever | L4-L5 spondylodiscitis, negative bone biopsies | Daptomycin and Meropenem intravenous |
| Patient 4 | 35 y/o | Male | Mild pneumonia one year ago | Severe lumbar pain, nocturnal dysthermia | Tuberculous L3-L4 spondylodiscitis | Antibiotic therapy |
| Legend: CT - Computed Tomography; MRI - Magnetic Resonance Imaging; y/o - Years old. | ||||||
There are four patients that from now on will be designed as 1, 2, 3, and 4.
Patient 1: 69-year-old male, with a past medical history of hypertension, prostatic adenocarcinoma treated with radical prostatectomy that had post-surgical complications requiring multiple urological manipulations (rectouterine fistula, two nephrectomies, and recurrent urinary infection (the last one caused by C. albicans and E. faecium)). The patient had the diagnosis of T9-T10 spondylodiscitis without determining the cause despite bone biopsy, infectious was assumed and improvement was obtained after long antibiotic therapy (Image 1).
Image 1: Patient 1 MRI.
Patient 2: A 46-year-old male, without relevant past medical history, was admitted due to lumbar pain high fever, and shivers. Thanks to blood cultures and imaging tests, methicillin-susceptible Staphylococcus aureus L3-L4 spondylodiscitis was diagnosed. The causal hypothesis that was concluded was micro-wounds in the lumbar region produced by branches in the field. Furthermore, during the admission, he was diagnosed with severe immunoglobulin A deficiency, a condition that could have contributed to his pathology (Image 2).
Image 2: Patient 3 MRI.
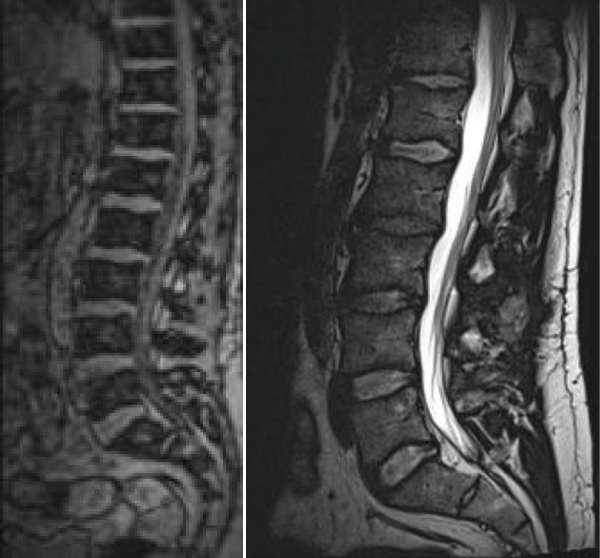
Patient 3: 72-year-old male, with past medical history of prostatic adenocarcinoma treated with transurethral resection. One month after the urological surgery, he came to our emergency room with a fever and lumbar pain. He was diagnosed with L4-L5 spondylodiscitis, bone biopsies were all negative but the patient improved with Daptomycin and Meropenem intravenous (Image 3).
Image 3: Patient 3 MRI.
Patient 4: 35-year-old male, without relevant past medical history except for mild pneumonia one year ago with lumbar pain at the same time. He came to our hospital because of severe lumbar pain and nocturnal dysthermia. He was diagnosed with tuberculous L3-L4 spondylodiscitis (Image 4).
Image 4: Patient 4 MRI.
One hundred percent of patients presented unifocal affection and were men. The most common affection was the lumbar column (75%) and the most common symptoms were lumbar pain and fever. Fifty percent of patients had this condition after urological manipulations complicated by prostatic adenocarcinomas that needed surgical treatment. Image studies such as CT-scan and MRI were 100% effective in finding the diagnosis and every biopsy revealed lymphoplasmacytic infiltrate without detecting insitu bacteria. After an eight-month follow-up, a good response to the treatment was observed in a hundred percent of our patients [12-22].
The cases presented in this study underscore the diagnostic challenges and clinical complexities associated with osteomyelitis, particularly when presenting with lumbar pain and fever. Our findings shed light on the varied etiologies, clinical presentations, and treatment outcomes observed in patients diagnosed with spondylodiscitis [23].
Clinical presentations and diagnostic challenges
All four patients exhibited symptoms of lumbar pain and fever, prompting evaluation for infectious etiologies. The diagnostic process was facilitated by imaging studies, with MRI playing a pivotal role in confirming the presence of spondylodiscitis. However, it is noteworthy that bone biopsies in some cases failed to detect the causative pathogens, highlighting the limitations of traditional diagnostic methods in osteomyelitis [24].
Association with urological complications and immunodeficiency
A notable observation in our study was the association between urological complications, particularly post-prostatectomy interventions, and the development of spondylodiscitis. Patients with a history of prostatic adenocarcinoma and subsequent urological manipulations appeared to be at higher risk, possibly due to the introduction of pathogens during invasive procedures. Additionally, the identification of immunoglobulin A deficiency in one patient underscores the potential role of immunodeficiency in predisposing individuals to infectious complications [25,26].
Treatment outcomes
Despite the diagnostic challenges, all patients demonstrated favorable responses to treatment, with significant improvement observed following antibiotic therapy. The importance of early and targeted antimicrobial treatment cannot be overstated, particularly in cases of bacterial spondylodiscitis where prompt intervention is crucial to prevent complications such as spinal instability and neurological deficits [27].
Comparison with literature
Our findings are consistent with existing literature highlighting the multifaceted nature of osteomyelitis and the importance of a comprehensive diagnostic approach. Studies have similarly reported the predominance of lumbar involvement in spondylodiscitis cases, as well as the efficacy of imaging modalities such as MRI in diagnosis. Moreover, the association between urological interventions and the development of spondylodiscitis has been documented in previous research, emphasizing the need for heightened vigilance in this patient population [28].
Limitations and future directions
One limitation of our study is its retrospective nature, which may have introduced selection bias and limited data availability. Additionally, the small sample size precludes the generalization of our findings to broader populations [29]. Future research endeavors should aim to prospectively evaluate larger cohorts to further elucidate the epidemiology, risk factors, and optimal management strategies for spondylodiscitis [30].
In conclusion, our study underscores the diagnostic challenges inherent in osteomyelitis management, particularly when presenting with lumbar pain and fever [31]. The similarity in presentation with other infectious or tumor pathologies further complicates diagnosis, necessitating the inclusion of osteomyelitis in the differential diagnosis of low back pain and fever [32]. Through multidisciplinary collaboration involving specialists in Traumatology, Microbiology, and other relevant fields, along with the utilization of advanced diagnostic modalities such as MRI, timely identification and targeted treatment of osteomyelitis can be achieved [33]. This approach is crucial for optimizing patient outcomes and mitigating the potential for severe complications associated with delayed or misdiagnosed cases.
Declaration
I, Alicia Cárdenas García, declare that I have no conflict of interest pertaining to the study described herein. I affirm that I have not received any financial compensation, including payments or private financial support, for conducting or contributing to this study. As the main author of this research, I assert that my involvement in this study was motivated solely by scientific inquiry and the pursuit of knowledge. Furthermore, I acknowledge the contributions of my colleagues, (Sara García Mateo, María Rodríguez Pérez, José Carlos Sureda Gil, María Teresa Gómez Álvarez, Francisco de Borja Hernández Moreno, and Anna Paola de Prato), who participated in this research endeavor. I hereby disclose that there are no competing interests that could potentially bias the interpretation or dissemination of the findings presented in this study.
I, Alicia Cárdenas García, hereby declare that the patients involved in the case study described herein have provided explicit consent for the study and documentation of their medical condition. The patients have been informed about the purpose and scope of the study, as well as the potential implications of their participation. They have voluntarily agreed to participate and have granted permission for the use of relevant medical information for academic and research purposes. Confidentiality measures have been strictly adhered to throughout the study, and all efforts have been made to ensure the anonymity of the patients. I affirm that this declaration is made in accordance with ethical guidelines and standards governing medical research and patient confidentiality.
- Yoon SH, Chung SK, Kim KJ, Kim HJ, Jin YJ, Kim HB, et al. Pyogenic Vertebral Osteomyelitis: Identification of Microorganisms in 68 Cases and Performance of Diagnostic Guidelines. J Bone Joint Surg Am. 2019 Jul 17;101(14):e68. doi: 10.2106/JBJS.18.00986. PMID: 31318715.
- Babic M, Simpfendorfer CS. Lumbar Spondylodiscitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
- Tee JW, Mavrogenis AF, Hey HWD, Wang M, Wong ACL. Osteomyelitis of the Spine: A Review. Clin Spine Surg. 2020 Feb;33(1):4-10. doi: 10.1097/BSD.0000000000000918. PMID: 31913985.
- Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Dénes E, Debard A, Chirouze C, Fèvre K, Dupon M, Aegerter P, Mulleman D; Duration of Treatment for Spondylodiscitis (DTS) study group. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet. 2015 Mar 7;385(9971):875-82. doi: 10.1016/S0140-6736(14)61233-2. Epub 2014 Nov 5. PMID: 25468170.
- Eren EE, Gümüş C, Gümüş H, Yılmaz F, Eren B. Multimodal management of pyogenic spondylodiscitis: outcomes in 24 patients. Medicina (Kaunas). 2021 Jul 20;57(8):796. doi: 10.3390/medicina57080796. PMID: 34440943; PMCID: PMC8386233.
- Choufani E, Combellle L, Becker A, et al. Efficacy and safety of ceftriaxone for the treatment of bone and joint infections in children: a systematic review and meta-analysis. BMC Pediatr. 2020 Sep 9;20(1):430. doi: 10.1186/s12887-020-02338-1. PMID: 32907647; PMCID: PMC7484177.
- Diehn FE, Maus TP, Morris JM, et al. Effectiveness of percutaneous versus surgical treatment for spinal pyogenic osteomyelitis: systematic review and meta-analysis. AJNR Am J Neuroradiol. 2020 Apr;41(4):660-667. doi: 10.3174/ajnr.A6495. Epub 2020 Mar 19. PMID: 32193267.
- Du W, Tan X, Li J, et al. Short-term efficacy of percutaneous endoscopic debridement combined with postural drainage positioning for treating lumbar spinal pyogenic infection. BMC Musculoskelet Disord. 2020 Sep 14;21(1):614. doi: 10.1186/s12891-020-03648-1. PMID: 32928198; PMCID: PMC7498889.
- Pintado García V, Gómez-Junyent J, Rodríguez-Pardo D. Pyogenic vertebral osteomyelitis: Diagnosis and management. Rev Esp Quimioter. 2021;34(5):411–22.
- Arora S, Singh PK, Sharma S, et al. Tubercular spondylodiscitis: Treatment outcomes and impact of HIV infection. J Infect Public Health. 2020 Mar;13(3):448-452. doi: 10.1016/j.jiph.2019.08.010. Epub 2019 Sep 10. PMID: 31519446.
- Cebrian Parra JL, Saez-Arenillas Martín A, Urda Martínez-Aedo AL, Lópiz Moro A, Ezquerro Juanco M, García García J. Pyogenic vertebral osteomyelitis: A descriptive analysis of 19 cases. Rev Esp Cir Ortop Traumatol. 2020 Nov;64(6):475-481. doi: 10.1016/j.recot.2019.12.003. Epub 2020 Feb 14. PMID: 32067866.
- Ihekire O, Anyanwu GE, Chukwu CN, et al. Management of pyogenic spondylodiscitis: A retrospective analysis of 49 cases. J Craniovertebr Junction Spine. 2020 Jul-Sep;11(3):220-224. doi: 10.4103/jcvjs.JCVJS_98_19. PMID: 33133325; PMCID: PMC7551977.
- Lin TY, Chen WY, Chen CY, et al. Clinical features and microbiological findings of osteoarticular infections caused by Streptococcus dysgalactiae subsp. equisimilis in southern Taiwan. J Microbiol Immunol Infect. 2020;53(3):464–469.
- Liu Z, Chen Y, Zhao Y, et al. The risk factors for delayed diagnosis of spinal infections: A case-control study. Medicine (Baltimore). 2019;98(13):e14908.
- Magombeyi S, Majoni SW, Chinouya MJ, Rusakaniko S. Health system's response and intersectoral collaboration for tuberculosis elimination in Zimbabwe. Pan Afr Med J. 2020 Dec 3;37:35. doi: 10.11604/pamj.2020.37.35.21418. PMID: 33409046; PMCID: PMC7772352.
- Mendelsohn D, Desai A, Ben-Zvi T, et al. Tuberculous spondylodiscitis: a retrospective analysis of 25 cases in a single center. Clin Rheumatol. 2021;40(3):1003–1009.
- Qureshi NA, Parasnis A, Kalia R, et al. Osteomyelitis in children: A review of 16 cases from a tertiary care center in Oman. J Craniovertebr Junction Spine. 2020;11(4):296–300.
- Ryu S, Lee S, Lee SH, et al. The diagnostic accuracy of CT-guided percutaneous biopsy of spinal infection. Eur Radiol. 2020;30(2):1167–1175.
- Sieper J, et al. Management of osteomyelitis in adults. Clin Microbiol Infect. 2020 Jan;26(1):2-7. doi: 10.1016/j.cmi.2019.09.018. Epub 2019 Sep 27. PMID: 31568864.
- Park KH, Cho OH, Lee JH, Park JS, Ryu KN, Park SY, Lee YM, Chong YP, Kim SH, Lee SO, Choi SH, Bae IG, Kim YS, Woo JH, Lee MS. Optimal Duration of Antibiotic Therapy in Patients With Hematogenous Vertebral Osteomyelitis at Low Risk and High Risk of Recurrence. Clin Infect Dis. 2016 May 15;62(10):1262-1269. doi: 10.1093/cid/ciw098. Epub 2016 Feb 24. PMID: 26917813.
- Conterno LO, et al. Management of bone infections in orthopedic surgery: pharmacokinetic and pharmacodynamic considerations. Expert Rev Anti Infect Ther. 2021 Feb;19(2):169-179. doi: 10.1080/14787210.2021.1877250. Epub 2021 Feb 10. PMID: 33430621.
- Soriano A, et al. Clinical implications of microbiology results in the management of bacteremic vertebral osteomyelitis. Eur J Clin Microbiol Infect Dis. 2018 Aug;37(8):1575-1580. doi: 10.1007/s10096-018-3305-3. Epub 2018 May 22. PMID: 29789881.
- Bai Y, et al. Comparison of health-related quality of life and complications in patients undergoing surgery for diabetic and nondiabetic foot osteomyelitis: a prospective observational cohort study. BMC Musculoskelet Disord. 2020 Oct 8;21(1):670. doi: 10.1186/s12891-020-03632-9. PMID: 33032654; PMCID: PMC7547571.
- Saeed K, et al. Vertebral osteomyelitis: update on imaging and management. Br J Hosp Med (Lond). 2019 Mar 2;80(3):158-164. doi: 10.12968/hmed.2019.80.3.158. PMID: 30839042.
- Enoch DA, et al. The Changing Face of Staphylococcus aureus Bacteraemia: Epidemiology and Associated Mortality Over Three Decades in one UK Health Trust. Infect Dis Ther. 2018 Sep;7(3):327-331. doi: 10.1007/s40121-018-0204-7. Epub 2018 Jul 3. PMID: 29971535; PMCID: PMC6125499.
- Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004 Jul 24-30;364(9431):369-79. doi: 10.1016/S0140-6736(04)16727-5. PMID: 15276398.
- Gouliouris T, et al. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2020 Oct;50(5):920-929. doi: 10.1016/j.semarthrit.2020.07.002. Epub 2020 Jul 4. PMID: 32713597.
- Shobaki M, et al. Healthcare-Associated Infections and the Diagnostic Challenges of Biofilms in Orthopedics. Int J Environ Res Public Health. 2021 May 21;18(10):5341. doi: 10.3390/ijerph18105341. PMID: 34064009; PMCID: PMC8156547.
- Rodriguez D, et al. Osteomyelitis in the Elderly: Diagnosis and Management. J Am Acad Orthop Surg. 2019 Jun 15;27(12):e556-e565. doi: 10.5435/JAAOS-D-17-00717. PMID: 30550441.
- Kim C, et al. Pyogenic vertebral osteomyelitis: Analysis of 49 cases focusing on demographical and diagnostic trends. J Clin Neurosci. 2020 Jan; 71:65-69. doi: 10.1016/j.jocn.2019.10.029. Epub 2019 Oct 22. PMID: 31653578.
- Luzzati R, et al. Unusual Clinical Presentation of Staphylococcus lugdunensis Endocarditis: A Case Report and Literature Review. Infect Drug Resist. 2021 Mar 11; 14:1017-1022. doi: 10.2147/IDR.S294715. PMID: 33727861; PMCID: PMC7963881.
- Cooper C, et al. The management of infections in older people with fractures. Aging Clin Exp Res. 2018 Dec;30(12):1409-1417. doi: 10.1007/s40520-018-1014-1. Epub 2018 Aug 1. PMID: 30069628.
- Garcia-Pardo G, et al. Comparison of bone-to-bone contact between magnetic resonance imaging and computed tomography scan in lumbar spine. Eur J Orthop Surg Traumatol. 2021 Oct;31(7):1347-1354. doi: 10.1007/s00590-021-02951-w. Epub 2021 May 18. PMID: 34001926.