More Information
Submitted: January 02, 2024 | Approved: January 29, 2024 | Published: January 30, 2024
How to cite this article: Szekelyi T, Lannes X, Jammal M, Qanadli SD, Wettstein M. Superior Gluteal Artery Pseudoaneurysm following a Periacetabular Osteotomy. Arch Clin Exp Orthop. 2024; 8: 001-004.
DOI: 10.29328/journal.aceo.1001018
Copyright Licence: © 2024 Szekelyi T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hip dysplasia; Periacetabular osteotomy; Vascular injury; Pseudoaneurysm; Embolization; Superior gluteal artery; Screw position
Superior Gluteal Artery Pseudoaneurysm following a Periacetabular Osteotomy
Tess Szekelyi1, Xavier Lannes2, Mouas Jammal3, Salah Dine Qanadli4 and Michael Wettstein5*
1Department of General Internal Medicine (SMIG), University Hospital of Geneva (HUG), Geneva, Switzerland
2Department of Orthopaedic Surgery, University Hospital of Lausanne (CHUV), Lausanne, Switzerland
3Department of Orthopaedic Surgery, Hôpital Intercantonal de la Broye (HIB), Payerne, Switzerland
4University Hospital of Lausanne, Lausanne, Switzerland; Riviera-Chablais Hospital HRC, Rennaz, Switzerland; Clinical Research Unit Riviera-Chablais Hospital HRC, Rennaz, Switzerland
5Medical Center ITOLS, Lausanne; Department of Orthopaedic Surgery, HRC – Riviera-Chablais Hospital HRC, Rennaz, Switzerland; Medical and Pharmacy Faculty of Laayoune, University Ibn Zohr, Agadir, Morocco
*Address for Correspondence: Michael Wettstein MD, Prof. Institute of Traumatology and Orthopaedics of Léman Suisse ITOLS Av. Théâtre 1 1005 Lausanne, Switzerland, Email: [email protected]
Periacetabular Osteotomy (PAO) is the gold standard for the treatment of hip dysplasia or acetabular retroversion. Due to the proximity of intra-pelvic arteries, there is a risk of iatrogenic vascular injuries, which can present with a delay and should be part of the differential diagnosis of significant pain following a PAO.
We present the case of a never-described vascular injury following a periacetabular osteotomy in a 25-year-old woman who presented with gluteal pain 3 weeks after surgery. A delayed diagnosis of a pseudoaneurysm of the superior gluteal artery was made and successfully treated by embolization. The lesion is most probably related to the tip of a screw or to the drilling process.
Acetabular reorientation by a so-called Periacetabular Osteotomy (PAO) has become the gold standard for treating Developmental Dysplasia of the Hip (DDH) or acetabular retroversion after physeal closure of the triradiate cartilage. The technique was described by Ganz, et al. in 1988 [1]. Some technical refinements were introduced over time, mainly concerning the surgical approach, but the basic technique of osteotomies, reorientation, and fixation has not changed since this first description.
However, PAO is a challenging surgery, with a steep learning curve reflected by a major complication rate ranging from 6% to 37% [2]. Vascular complications account for 2.3% as reported in a recent review [3]. Arterial complications have rarely been reported, but the potential danger to internal iliac vessels and their branches has been highlighted by a few case reports [4,5] and cadaveric studies [6,7].
Pseudoaneurysms of the superior gluteal artery are extremely rare, however, they are more frequent than inferior gluteal artery pseudoaneurysms [8]. They are usually related to pelvic trauma, penetrating wounds, local inflammation, or infection [9]. Iatrogenic cases have been reported after intramedullary nailing of femoral fractures, iliac pelvic screw fixation for spinal deformity, pelvic stabilization using a C-clamp or iliosacral screw fixation, bone marrow biopsy, or revision total hip arthroplasty [10-17]. Usually, direct sharp contact with the pulsatile artery induces a dissection of the arterial wall, leading to the formation of a blood-filled bag, enveloped only by the outer part of the arterial wall, or adventitia. Excepted the mass effect of the pseudoaneurysm which can be painful, it can also rupture, causing acute bleeding [18].
We report the case of a superior gluteal artery pseudoaneurysm following a PAO for DDH in a 25-year-old patient. To our knowledge, this is the first description of such an injury following a PAO.
Consent was obtained from the patient before publication.
An otherwise healthy 25-year-old female patient, known for lumbar pain related to Scheurmann’s disease, developed left hip pain in the context of a bilateral severe developmental dysplasia, which was asymptomatic on the right side. She was treated with a left periacetabular reorientation osteotomy with a simultaneous cervico-cephalic offset correction, performed by an experienced hip surgeon. A minimal-invasive anterior approach with a “Bikini” incision was performed followed by ischial, pubic, and iliac osteotomies to allow for a complete mobilization of the acetabular fragment, which was reoriented before definitive fixation using three 3.5 millimeter cortical screws in a usual triangular way. Fluoroscopic controls during surgery were satisfactory and showed no complications. Because of a restriction in internal rotation, an arthrotomy was performed to correct the deficient anterior offset of the femoral head, using a T-shaped arthrotomy through the same approach.
The initial post-operative period was uneventful.
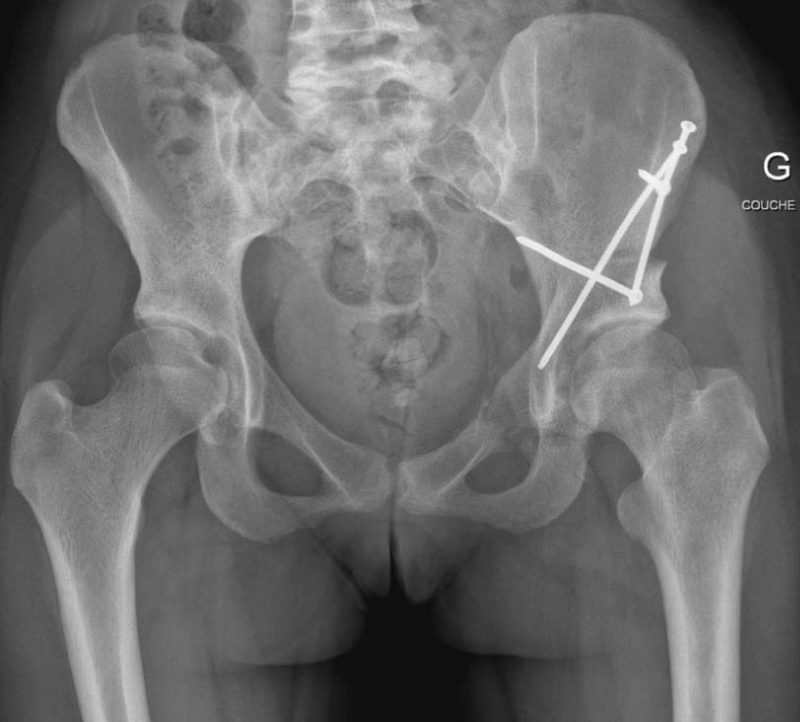
Three weeks after surgery, she presented in a level III emergency department with acute severe left gluteal pain. Clinical examination showed an already known lateral femoro-cutaneous hypoesthesia of the thigh, but no signs of inflammation of the scar or other neurological or vascular deficits. Laboratory data were normal. An antero-posterior pelvic X-ray and an axial left hip X-ray showed no secondary displacement of the acetabular fragment or the screws or any other complication (Figure 1). The diagnosis was a resurgence of pain after an increase in activity and the patient was released home with an adapted analgesic treatment.
Figure 1: Antero-posterior pelvic X-rays three weeks post-operative with no sign of secondary displacement of the fragment or screws or other complications.
One week later, she presented again with the same complaints without a traumatic event and a well-conducted analgesic treatment. The physical exam and laboratory tests were normal. A native pelvic computed tomography scan (CT scan) found a swelling around the left piriformis muscle with a discrete mass effect on surrounding tissues, which was considered a postoperative hematoma. Analgesic treatment was increased but was still insufficient as she returned the next day with uncontrolled pain and additionally, a sciatic pain irradiating from the left buttock to the calf.
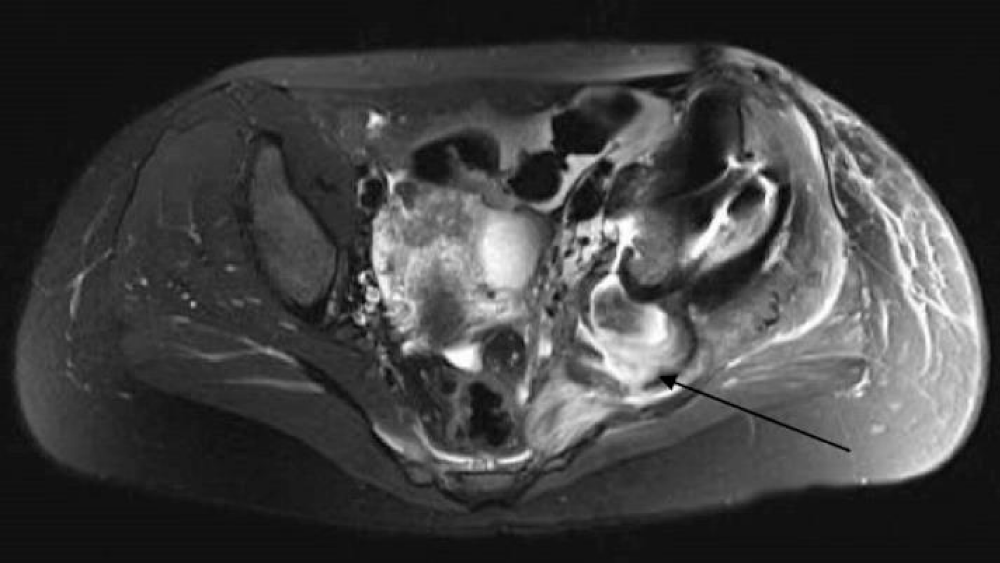
An outpatient examination by the surgeon concluded a possible lumbar implication or local sciatic compression. Lumbar and pelvic Magnetic Resonance Imaging (MRI) were obtained, showing no lumbar pathology but an important swelling of the left gluteus medius, piriformis, and internal obturator muscles. A mass effect behind the sciatic notch was identified and considered a hematoma (Figure 2).
Figure 2: Axial T2 view of the pelvic MRI showing swelling of the gluteus medius, piriformis, internal obturator, and iliac muscles on the left side. A mass effect can be seen behind the sciatic notch, interpreted as a hematoma (arrow).
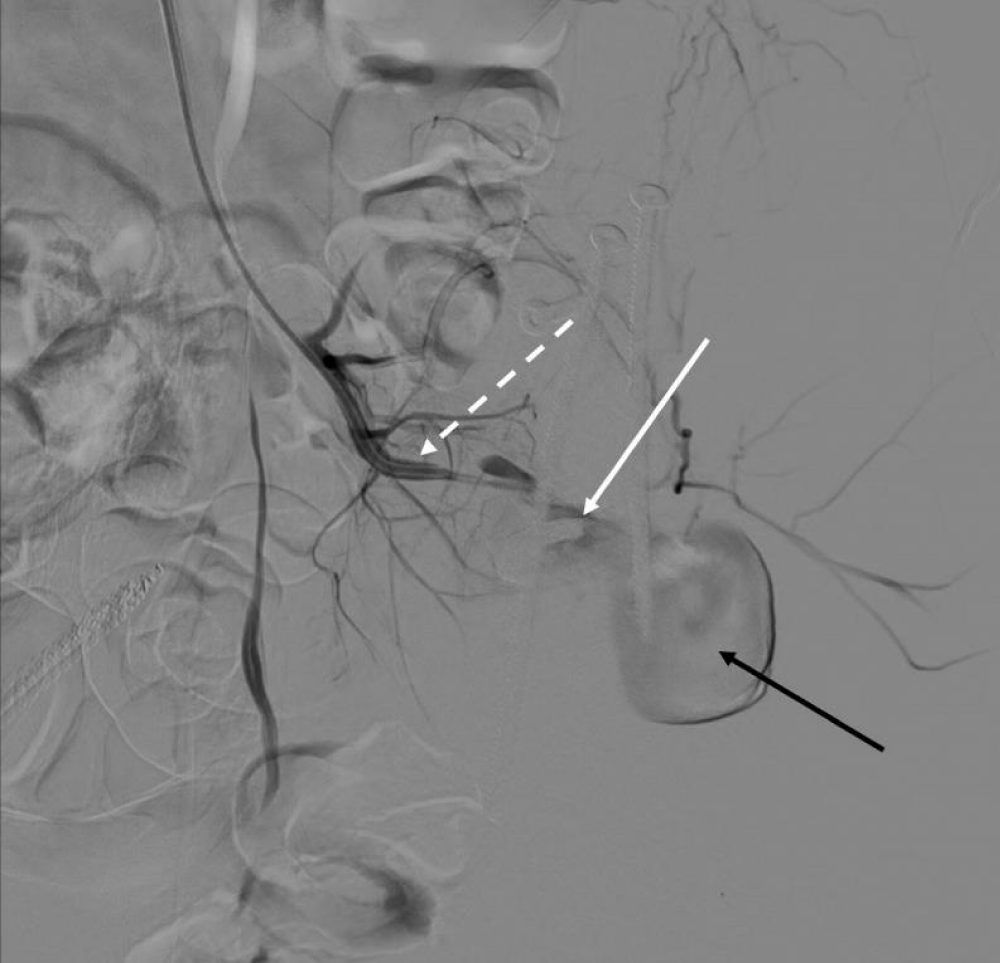
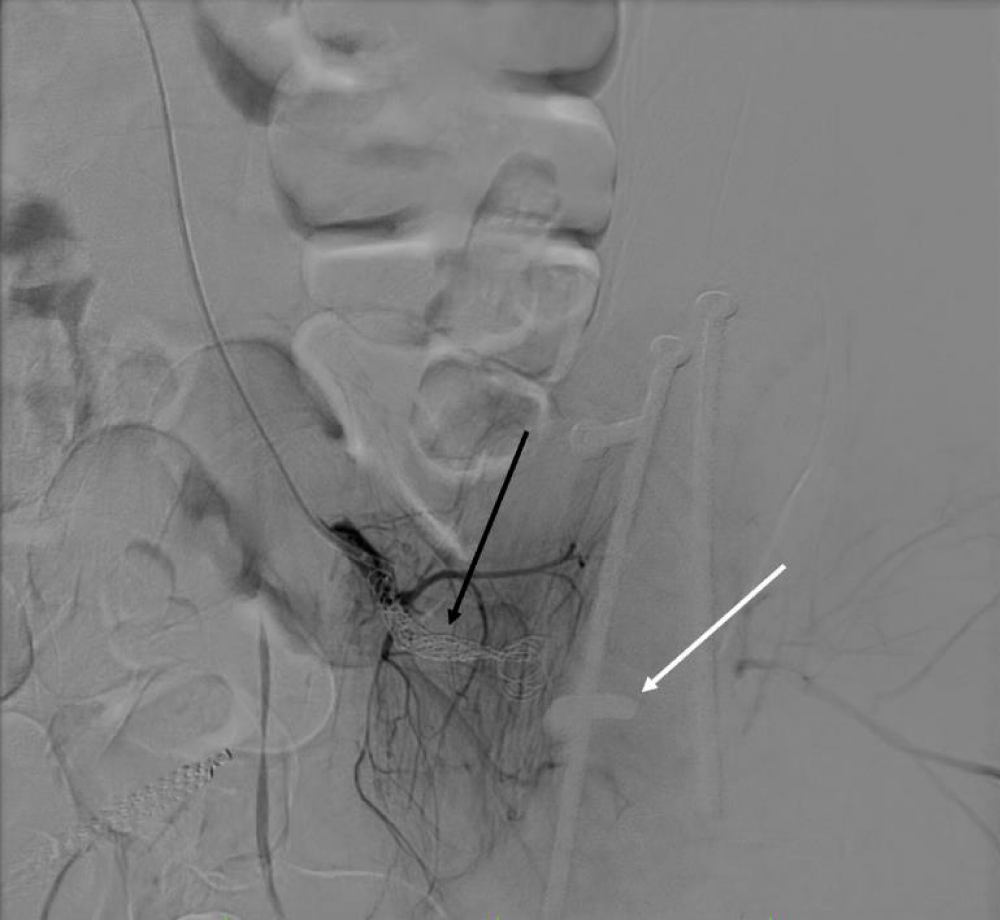
Finally, a pelvic CT scan after contrast agent injection was performed to search for vascular complications. This showed a pseudoaneurysm of the superior gluteal artery located just at the level of a screw tip in the sciatic notch (Figure 3). The patient then underwent embolization of the superior gluteal artery with coils in the Interventional Radiology Department of the local University Hospital, which led to a rapid resolution of symptoms (Figures 4a,b).
Figure 3: Axial view of a contrast pelvic CT scan showing a mass effect starting from the superior gluteal artery and diagnosed as a pseudoaneurysm (black arrow). The white arrow shows the close proximity of the antero-posterior screw tip to the artery.
Follow-up at 4 months after surgery showed a complete healing of the osteotomy, good muscle function, and no further complications or symptoms.
Figure 4a: Subtraction image from the selective angiography of the left superior gluteal artery (interrupted white arrow) showing the pseudoaneurysm (black arrow) before embolization. The white arrow shows the tip of the antero-posterior screw in close contact with the superior gluteal artery.
Figure 4b: Subtraction image after coiling of the superior gluteal artery (black arrow), showing no residual pseudoaneurysm at the tip of the antero-posterior screw (white arrow).
PAO is an effective treatment to correct symptomatic acetabular dysplasia or retroversion by reorienting the acetabulum and seems to significantly delay the need for total hip arthroplasty in well-selected patients [1,2,19].
Complications of PAO, described as major and minor in the literature, are noteworthy. Clohisy et al. reported major complications, including vascular complications, ranging from 6% to 37% on 13 selected original case series including a total of 626 PAOs in 566 patients [2]. A review including more than 2000 cases of PAO found that 2.3% of the cases presented vascular complications, including hematoma and major blood loss during surgery [3]. There have been two reports of obturator artery injury during a PAO, and both seem to have occurred when the pubic osteotomy was performed [4,5]. Cadaveric studies described how to avoid obturator artery injury during pubic and ischial osteotomy performed during PAO [7], and described the acetabular blood supply and its implication for PAO [6]. However, to our knowledge, no case of superior gluteal artery injury has been reported and no cadaveric studies performed to estimate its safeness during PAO.
In cases with unexplained pain after a major hip or pelvic surgery, a high suspicion index should be kept for soft tissue or bony lesions. In this context, a CT scan of the hip should be considered as the complex anatomy of the pelvis may hide some structural abnormalities on standard X-rays. This imaging modality allows for control for eventual fractures, bone spikes, osteosynthesis material malposition, or other complications, as well as other pathologies of the close-lying gastrointestinal, urogenital, or gynecological structures [20]. The use of imaging after contrast agent injection, specifically CTangiography, can highlight vascular complications, such as hematomas or active bleeding as well as any other vascular lesions and give topographic information [9].
The superior gluteal artery is a branch of the internal iliac artery exiting the sciatic notch above the piriformis muscle, in close contact with the bone, to vascularize the gluteal muscles. The possibility of an anatomical variation of the intra-pelvic arteries was excluded in this case.
A pseudoaneurysm of the superior gluteal artery is extremely rare and diagnosis is difficult because of an aspecific clinical presentation and possible delayed presentation from the original injury. Taif and al. described a case of such an injury after a car accident with a left acetabular fracture treated conservatively, which presented with a painful swollen gluteal mass with radiation and numbness to the lower limb two years after the trauma [21]. The diagnosis was delayed because sciatic pain symptoms masked the arterial etiology, as in the present case. Nachbur et al. describe several mechanisms for arterial injury in hip surgery such as repeated trauma by screws, osteophytes, or cement that entered the pelvis during surgery [22].
In our case, the CT scan (Figure 3) as well as the angiography showed a very close contact between the tip of one of the screws and the pseudoaneurysm (Figure 4a). We hypothesize that the injury occurred either during the drilling process or because of an irritation of the artery by the screw tip, provoking the formation of a pseudoaneurysm which explains the increasing mass effect on the sciatic nerve causing neuralgic pain in the leg [22]. This problem is due to a rather horizontal orientation of the anteroposterior screw, which is usually oriented more proximally towards the sacro-iliac joint. This orientation cannot be considered as wrong, but due to our present experience, we recommend aiming the drill bit more vertically, as the screw tip can overlap the opposite cortical bone, and could thus put nearby neurovascular structures at risk of acute or delayed injury if it is located in the sciatic notch.
To our knowledge, this case is the first report of an iatrogenic pseudoaneurysm of the superior gluteal artery following PAO.
Besides the symptoms related to local compression, as in our case, arterial pseudoaneurysms may rupture at any time and cause acute pain related to the hematoma or even a potentially life-threatening hemorrhage and therefore represent a medical emergency. Endovascular embolization is the treatment of choice.
According to the literature, the obturator artery is most likely to be injured during PAO, but injuries to other vessels may always happen. A delayed presentation of such injuries is typical and should therefore be kept in mind. In case of atypical pain, we suggest that a CT scan or MRI with contrast agent injection and vascular sequences should be included in the workup.
- Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988 Jul;(232):26-36. PMID: 3383491.
- Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009 Aug;467(8):2041-52. doi: 10.1007/s11999-009-0842-6. Epub 2009 Apr 21. PMID: 19381741; PMCID: PMC2706361.
- Swarup I, Ricciardi BF, Sink EL. Avoiding Complications in Periacetabular Osteotomy. JBJS Rev. 2015 Nov 24;3(11):e4. doi: 10.2106/JBJS.RVW.O.00023. PMID: 27490913.
- Toki S, Nagamachi A, Yonezu H, Adachi K, Inoue K, Naito M. Injury to the Obturator Artery During Periacetabular Osteotomy: A Case Report. JBJS Case Connect. 2016 Jan-Mar;6(1):e9. doi: 10.2106/JBJS.CC.O.00078. PMID: 29252715.
- Brenoe AS, Andersen PE, Overgaard S. [Endovascular embolisation of severe bleeding in connection with periacetabular osteotomy]. Ugeskr Laeger. 2006; 168: 14531454.
- Beck M, Leunig M, Ellis T, Sledge JB, Ganz R. The acetabular blood supply: implications for periacetabular osteotomies. Surg Radiol Anat. 2003 Nov-Dec;25(5-6):361-7. doi: 10.1007/s00276-003-0149-3. Epub 2003 Aug 16. PMID: 12923665.
- Kamada S, Naito M, Shiramizu K, Nakamura Y, Kinoshita K. Is the obturator artery safe when performing ischial osteotomy during periacetabular osteotomy? Int Orthop. 2011 Apr;35(4):503-6. doi: 10.1007/s00264-010-1064-y. Epub 2010 Jun 16. PMID: 20556381; PMCID: PMC3066328.
- Agarwal M, Giannoudis PV, Syed AA, Hinsche AF, Matthews SJ, Smith RM. Pseudoaneurysm of the inferior gluteal artery following polytrauma: diverse presentation of a dangerous complication: a report of two cases. J Orthop Trauma. 2003 Jan;17(1):70-4. doi: 10.1097/00005131-200301000-00013. PMID: 12499973.
- Romero L, Serrallé C, Fernández Noya J, González P, Mosquera NJ. Superior Gluteal Artery Pseudoaneurysm: Two Cases Report and Review of the Literature. Port J Card Thorac Vasc Surg. 2021 Nov 7;28(3):47-49. doi: 10.48729/pjctvs.194. PMID: 35333469.
- Ailaney N, O'Connell R, Giambra L, Golladay G. Superior gluteal artery pseudoaneurysm following intramedullary nailing of an atypical femoral fracture. BMJ Case Rep. 2019 Oct 23;12(10):e231490. doi: 10.1136/bcr-2019-231490. PMID: 31645404; PMCID: PMC6827729.
- Khela M, Kasir R, Lokken RP, Clark AJ, Theologis AA. Bilateral dual iliac screw pelvic fixation for adult spinal deformity: a case report of a superior gluteal artery pseudoaneurysm secondary to aberrant iliac screw trajectory. Spine Deform. 2023 Oct 26. doi: 10.1007/s43390-023-00774-y. Epub ahead of print. PMID: 37882967.
- Kim WY, Lee SW, Kim KS, Lee JY. Superior Gluteal Artery Pseudoaneurysm Caused by Pelvic C-Clamp Blind Application: A Case Report. Hip Pelvis. 2017 Jun;29(2):145-149. doi: 10.5371/hp.2017.29.2.145. Epub 2017 Jun 2. PMID: 28611967; PMCID: PMC5465397.
- Maled I, Velez R, Lopez R, Batalla L, Caja VL. Pseudoaneurysm of the superior gluteal artery during iliosacral screw fixation. Acta Orthop Belg. 2007 Aug;73(4):544-7. PMID: 17939491.
- Stavrakakis IM, Magarakis GE, Liodakis G, Tavlas E, Tsetis DK. Sciatic Nerve Palsy due to a Superior Gluteal Artery Pseudoaneurysm PostBone Marrow Biopsy: A Case Report and Review of the Literature. J Orthop Case Rep. 2018 Jul-Aug;8(4):74-77. doi: 10.13107/jocr.2250-0685.1168. PMID: 30687669; PMCID: PMC6343557.
- Sullivan CM, Regi JM. Pseudoaneurysm of the superior gluteal artery following bone marrow biopsy. Br J Haematol. 2013 Apr;161(2):289-91. doi: 10.1111/bjh.12216. Epub 2013 Jan 29. PMID: 23356434.
- Slullitel PA, Llano L, García-Ávila C, Diaz-Dilernia F, Piccaluga F, Buttaro M, Zanotti G, Comba F. Unaddressed arterial injuries in revision total hip arthroplasty: mortality outcomes of a low-prevalence complication. Int Orthop. 2020 Jan;44(1):23-29. doi: 10.1007/s00264-019-04358-2. Epub 2019 Jun 20. PMID: 31222421.
- Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997 Jul;43(1):146-9. doi: 10.1097/00005373-199707000-00037. PMID: 9253929.
- Rivera PA, Dattilo JB. Pseudoaneurysm. In StatPearls; Treasure Island (FL). 2024.
- Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008 Jul;466(7):1633-44. doi: 10.1007/s11999-008-0242-3. Epub 2008 May 1. PMID: 18449617; PMCID: PMC2505253.
- Shetty M. Acute Pelvic Pain: Role of Imaging in the Diagnosis and Management. Semin Ultrasound CT MR. 2023 Dec;44(6):491-500. doi: 10.1053/j.sult.2023.10.004. Epub 2023 Oct 12. PMID: 37832696.
- Taif S, Derweesh A, Talib M. Superior gluteal artery pseudoaneurysm presenting as a gluteal mass: case report and review of literature. J Clin Imaging Sci. 2013 Oct 29;3:49. doi: 10.4103/2156-7514.120805. PMID: 24228217; PMCID: PMC3823385.
- Nachbur B, Meyer RP, Verkkala K, Zürcher R. The mechanisms of severe arterial injury in surgery of the hip joint. Clin Orthop Relat Res. 1979 Jun;(141):122-33. PMID: 477093.