More Information
Submitted: May 31, 2023 | Approved: June 13, 2023 | Published: June 14, 2023
How to cite this article: Tade Yanick S, Liu John L, Pirela Cruz MA. Treatment of a Distal Humerus Fracture using an Elbow Hemiarthroplasty. Arch Clin Exp Orthop. 2023; 7: 018-021.
DOI: 10.29328/journal.aceo.1001016
Copyright Licence: © 2023 Tade Yanick S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Elbow hemiarthroplasty; Distal humeral replacement; Ulnohumeral joint
Treatment of a Distal Humerus Fracture using an Elbow Hemiarthroplasty
Tade Yanick S*, Liu John L and Miguel A Pirela Cruz
Creighton University School of Medicine, USA
*Address for Correspondence: Tade Yanick S, Creighton University School of Medicine, USA, Email: [email protected]
Elbow hemiarthroplasty (EHA) is a highly effective procedure for treating various elbow joint disorders such as rheumatoid arthritis, osteoarthritis, and fractures involving the articular surface of the distal humerus. It involves replacing the entire distal humerus with a prosthesis and reattaching the supporting soft tissues. The EHA provides significant pain relief, improves joint function, and increases patient satisfaction, with minimal complications that can be easily managed. This case study demonstrates the value of EHA as a viable treatment option for distal humerus fractures in older adults with moderate activity levels, as a superior alternative to osteosynthesis.
Fractures of the distal humerus, particularly in the elderly population, are a challenging clinical entity that can significantly impact the quality of life [1,2]. Different treatment options have been used including open reduction and internal fixation, which is the standard approach for these injuries, total elbow arthroplasty, and resection arthroplasty with facial interposition [3]. Severe articular destruction coupled with osteoporosis further raises the level of complexity in the management of these fractures. Hemi-arthroplasty of the elbow is a surgical approach that involves replacing only the humeral side of the elbow joint, leaving the ulna side intact. Despite the growing popularity of this procedure, there is still a lack of consensus regarding humeral hemi-arthroplasty in managing distal humerus fractures [4-6]. This paper aims to provide a comprehensive review of the available literature on hemi-arthroplasty for distal humerus fractures and to demonstrate the benefits of this surgical approach. We will examine the outcomes of this surgical approach in terms of pain relief, restoration of function, range of motion, and complications. The study will provide additional insights into the effectiveness of hemi-arthroplasty of the elbow for distal humerus fractures, which can aid in improved clinical decision-making and patient care.
Informed consent was obtained from the patient for treatment and teaching purposes. The patient is a 71-year-old female, with a few comorbidities but a history of osteoporosis. Who presented to the emergency department to evaluate left upper extremity pain. She gave a history of a ground-level fall that occurred just before her arrival and related to accidentally tripping and striking her left elbow against the ground. She denies hitting her head or losing consciousness and did not have any additional injuries. The patient reported experiencing constant pain in her left elbow that was exacerbated by elbow movement. She denied chest pain, neck pain, or back pain and was otherwise healthy.
During the physical examination, we found swelling and tenderness around the patient’s left elbow. There were no cuts or scrapes on the skin. The elbow’s active and passive range of motion was impossible due to pain and protective guarding. The patient also experienced mild discomfort over their left distal radius, but there was no visible deformity. The range of motion in their left wrist was normal, and there was no tenderness in their left shoulder. We found no abnormalities in the right upper or lower extremities. The patient’s neurological examination of the left upper extremity was normal for the musculocutaneous, radial, ulnar, and median nerves.
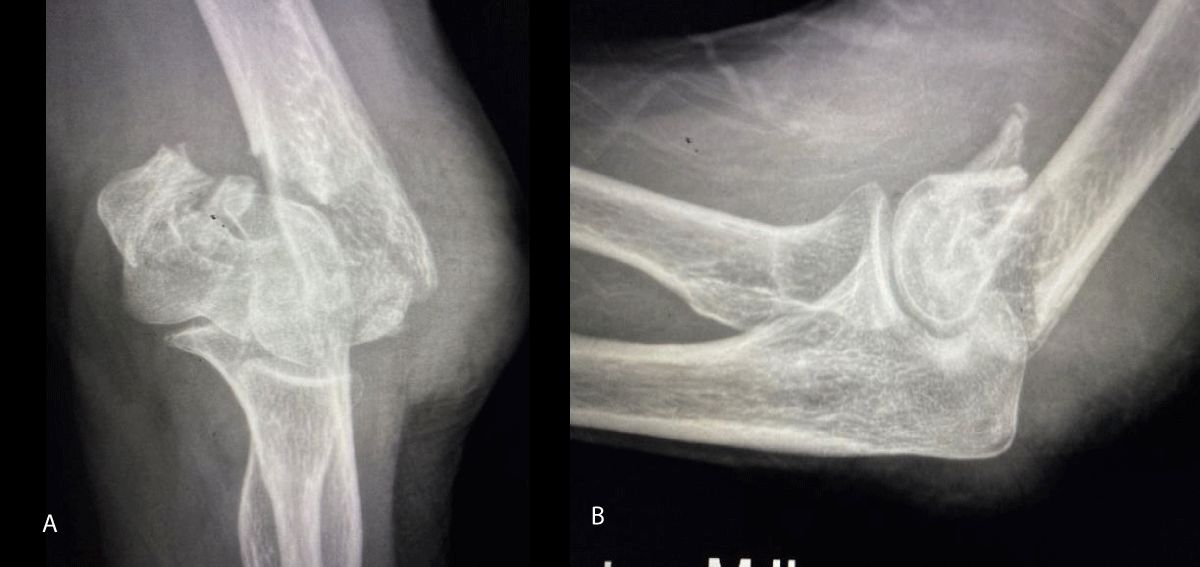
Radiographs of the left elbow included a PA and lateral and oblique projections, demonstrated severely displaced, comminuted, and intra-articular fractures trochlea and capitellum of the distal humerus (Figures 1,2). The patient was also noted to have generalized osteopenia.
Figure 1: A and B: Demonstrates PA and Lateral injury radiographs of the patient.
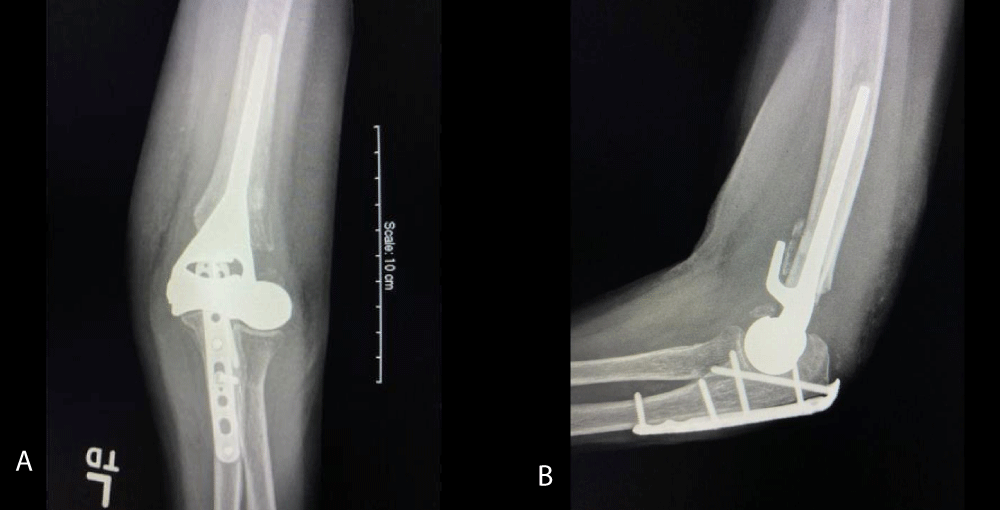
Figure 2: A and B: Are the radiographs 2 weeks after surgery.
ospital course
In the ED, after her initial evaluation, an orthopedic consultation was obtained and the patient underwent an attempt at closed reduction of the fracture and application of a splint for immobilization. A detailed CT scan was obtained of the left elbow which included a 3D reconstruction of the injury for further scrutiny.
Various treatment options were discussed with the patient which included nonoperative and operative options. For this patient, we felt that early surgical intervention was in her best interest. Due to the nature of her injury, her history of osteoporosis, and the fact that this was her nondominant extremity, we felt that a hemiarthroplasty was in her best interest which would allow for early return of function and pain relief.
The following day, the patient was taken to the operating room and a hemiarthroplasty of the left elbow was performed. “The primary indication for elbow hemi arthroplasty (EHA) based on the bulk of the literature is an un-reconstructable acute distal humeral fracture in an older active patient” [7]. This decision is best made intra-operatively.
Technique and intraoperative decision making
An inter-scalene regional block was obtained for the extremity and a general anesthetic was established. The patient was placed into a lateral position, allowing easy access to the image intensifier for intraoperative X-rays. A posterior approach to the elbow was performed after the tourniquet was elevated. The ulnar nerve was dissected out and away from the cubital tunnel and protected with a Penrose drain. A chevron osteotomy was performed to allow for reflection of the triceps tendon and the extensor mechanism of the elbow. After the triceps tendon was reflected, the comminuted distal humerus was exposed. A careful evaluation was performed at this time to determine if an open reduction and internal fixation were an option. Still, as the initial radiographs demonstrated, the hemiarthroplasty was a better option for this patient. The fracture fragments were removed in a piecemeal fashion. The collateral ligaments were tagged for easy identification. A transverse osteotomy was performed just above the level of the olecranon fossa with an oscillating saw. The humeral canal was then prepared for prosthesis. The level of the prosthesis was also determined. This is critical to restore normal myofascial tension for the musculature of the elbow. After the appropriate broaching and reaming, the humeral trial was inserted, and intraoperative X-rays were obtained. Final adjustments are made as necessary. The ulna lateral collateral and medial collateral ligaments are tagged with Fiber wire suture. The actual prosthesis is then inserted after the wound has been irrigated thoroughly. Cement is used to set the prosthesis at the appropriate height. The collateral ligaments are attached to the center of rotation. Additional supplemental sutures are placed along the pillars of the prosthesis for additional support and stabilization of the soft tissue sleeve. The osteotomy is then repaired with either plate or tension band fixation.
Postoperative course
A short course of immobilization for 2 to 3 weeks with the elbow at approximately 90 degrees is appropriate. A range of motion and rehabilitation program is then initiated.
The patient attended occupational therapy frequently to work on a range of motion, reduce the pain and improve the function of the left upper extremity.
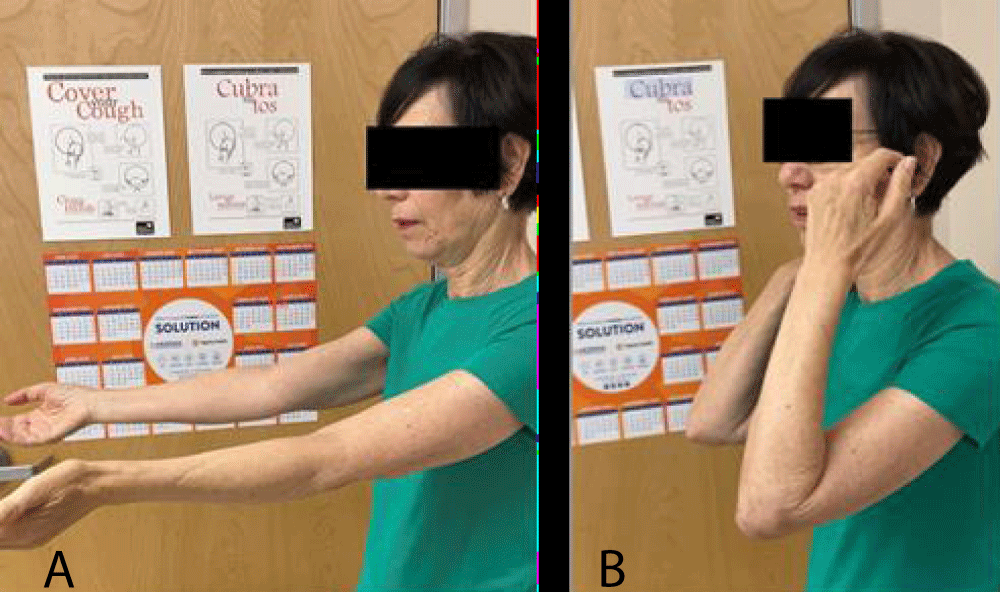
A year after the procedure was performed, she was noted to be able to extend her elbow to 0 degrees and flex to 130 degrees, actively. She has full pronation and full supination. The patient was pain-free with no signs of instability and could perform her usual activities of daily living. She was given a permanent lifting restriction of 15 – 20 lbs Figures 3,4.
Figure 3: A and 3B: Show the patient’s final flexion and extension of her left elbow.
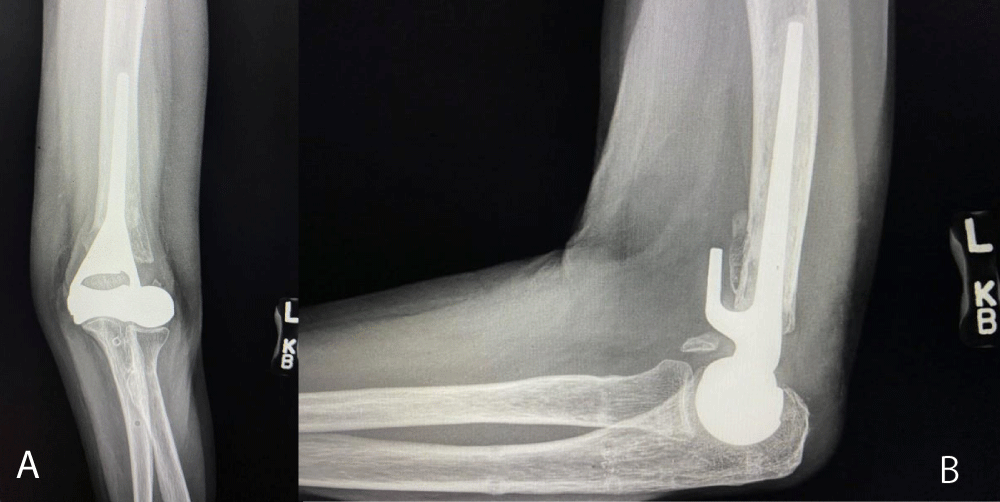
Figure 4: A and B: Radiographs at one-year post-op demonstrate the prosthesis is stable with no signs of loosening and the ulna chevon osteotomy is healed.
Pulmonary nodules: One of 10 mm in the right lung, it can be a hamartoma, granuloma, or metastasis; and several millimeters in the lingula, probable granulomas and less probable metastasis.
Various treatment options have been used to address fractures of the distal humerus in the elderly population as far back as the 1940 s and 1950 s including non-operative treatment, which involves immobilization and range of motion to restore function [8-10]. Operative treatments include open reduction and internal fixation, which is the time and true gold standard for managing these injuries [5]. Total elbow replacement is another consideration that is commonly used in elderly patients [6]. Arthrodesis and resection arthroplasty with or without facial (or other) interposition are salvage procedures that are rarely employed but may be a reasonable option in complex cases such as infection [11,12].
Distal humerus fractures are common injuries in the elderly population, and these fractures can significantly impact the quality of life. Treating these fractures is often challenging, and the optimal management strategy remains controversial. Although osteosynthesis has been the gold standard recently, hemiarthroplasty has emerged as a viable surgical option for elderly patients with fractures involving the articular surface of the distal radius.
Hemiarthroplasty of the elbow involves the replacement of the distal humerus, leaving the ulna relatively intact (without a prosthesis). The procedure can be performed with or without an olecranon osteotomy. The primary benefit of this procedure is that it provides immediate pain relief and restores joint function [13]. Moreover, it avoids an early range of motion after a short period of immobilization, which helps to prevent complications such as stiffness with a limited range of motion [14].
Studies have shown that hemiarthroplasty provides excellent pain relief and functional outcomes in elderly patients with distal radius fractures involving the articular surface [11,15,16]. In a recent study, patients who underwent hemiarthroplasty had significantly better wrist function and range of motion than those who underwent other surgical procedures. Moreover, they reported higher overall satisfaction with their recovery. Studies also showed that hemiarthroplasty had a lower complication rate than total joint replacement.
There is a distinction that needs to be made between ulnohumeral hemiarthroplasty and distal humeral replacement. Both terms have been used interchangeably throughout the literature, still the former involves retention or preservation of the epicondylar region of the distal humerus and the latter involves a more proximal resection with excision of these structures. In this clinical case, the distal humerus was replaced with reattachment of the surrounding soft tissues the supporting collateral ligaments.
There are ethical considerations that need to be addressed. Although hemiarthroplasty and distal humeral replacement procedures have been used clinically, this procedure is considered to be an off-label procedure since it has not been approved by the Food and Drug Administration (FDA). Special consent needs to be obtained from the patient before performing the surgery. The option to perform an EHA must be reserved for the surgeon intraoperatively. If fixation is noted to be suboptimal, then consideration for performing the hemiarthroplasty should be considered. Moreover, preoperative evaluation including radiographs and details CT studies do not always give a complete clinical picture. Some factors are not immediately apparent, and therefore it is important for the surgeon to be prepared to perform this procedure as a salvage option if needed. The advantage of surgery is to preserve the bone stock and to improve the functionality of the elbow and upper extremity before the patient requires a total elbow replacement which has severe post-operative restrictions such as lifting no more than 2 pounds for the upper extremity. Generally speaking, we place a weight-lifting restriction on the patients to no more than 10 pounds for the upper extremity after this procedure.
In conclusion, hemiarthroplasty is a viable surgical option for elderly patients with distal humerus fractures involving the articular surface when osteosynthesis is not possible i.e., an un-reconstructable fracture. It provides immediate pain relief and restores joint function while avoiding the need for extensive surgery involving the ulna. While total elbow replacement may be appropriate for more severe injuries or pre-existing degenerative joint disease, hemiarthroplasty provides another option with a low complication rate.
- Varecka TF, Myeroff C. Distal Humerus Fractures in the Elderly Population. J Am Acad Orthop Surg. 2017 Oct;25(10):673-683. doi: 10.5435/JAAOS-D-15-00683. PMID: 28953082.
- Palvanen M, Kannus P, Niemi S, Parkkari J. Secular trends in the osteoporotic fractures of the distal humerus in elderly women. Eur J Epidemiol. 1998 Feb;14(2):159-64. doi: 10.1023/a:1007496318884. PMID: 9556175.
- Seok HG, Park JJ, Park SG. Comparison of the Complications, Reoperations, and Clinical Outcomes between Open Reduction and Internal Fixation and Total Elbow Arthroplasty for Distal Humeral Fractures in the Elderly: A Systematic Review and Meta-Analysis. J Clin Med. 2022 Sep 29;11(19):5775. doi: 10.3390/jcm11195775. PMID: 36233648; PMCID: PMC9571352.
- Phadnis J, Watts AC, Bain GI. Elbow hemiarthroplasty for the management of distal humeral fractures: current technique, indications and results. Shoulder Elbow. 2016 Jul;8(3):171-83. doi: 10.1177/1758573216640210. Epub 2016 Apr 21. PMID: 27583016; PMCID: PMC4950283.
- Jukes CP, Dirckx M, Phadnis J. Current concepts in distal humeral hemiarthroplasty. J Clin Orthop Trauma. 2021 May 27;19:224-230. doi: 10.1016/j.jcot.2021.05.025. PMID: 34150495; PMCID: PMC8190472.
- Rangarajan R, Papandrea RF, Cil A. Distal Humeral Hemiarthroplasty Versus Total Elbow Arthroplasty for Acute Distal Humeral Fractures. Orthopedics. 2017 Jan 1;40(1):13-23. doi: 10.3928/01477447-20161227-02. PMID: 28375524.
- Jukes CP, Dirckx M, Phadnis J. Current concepts in distal humeral hemiarthroplasty. J Clin Orthop Trauma. 2021 May 27;19:224-230. doi: 10.1016/j.jcot.2021.05.025. PMID: 34150495; PMCID: PMC8190472.
- Mellen RH, Phalen GS. Arthroplasty of the elbow by replacement of the distal portion of the humerus with an acrylic prosthesis. J Bone Joint Surg Am. 1947 Apr;29(2):348-53. PMID: 20240192.
- VenablE CS. An elbow and an elbow prosthesis; case of complete loss of the lower third of the humerus. Am J Surg. 1952 Mar;83(3):271-5. doi: 10.1016/0002-9610(52)90255-9. PMID: 14903376.
- Macausland WR. Replacement of the lower end of the humerus with a prosthesis; a report of four cases. West J Surg Obstet Gynecol. 1954 Nov;62(11):557-66. PMID: 13217249.
- Celli A, Ricciarelli M, Guerra E, Bonucci P, Ritali A, Cavallo M, Rotini M, Rotini R. Elbow hemiarthroplasty for acute distal humeral fractures and their sequelae: medium- and long-term follow-up of 41 cases. J Shoulder Elbow Surg. 2022 May;31(5):1015-1025. doi: 10.1016/j.jse.2021.12.030. Epub 2022 Jan 26. PMID: 35091072.
- Street DM, Stevens PS. A humeral replacement prosthesis for the elbow: results in ten elbows. J Bone Joint Surg Am. 1974 Sep;56(6):1147-58. PMID: 4436351.
- Chang N, King GJW. Elbow Hemiarthroplasty for the Treatment of Distal Humerus Fractures. Orthop Clin North Am. 2020 Apr;51(2):265-277. doi: 10.1016/j.ocl.2019.11.009. Epub 2020 Feb 3. PMID: 32138864.
- Stone A, Chan G, Sinclair L, Phadnis J. Elbow arthroplasty in trauma-current concepts review. J Orthop. 2022 Nov 23;35:126-133. doi: 10.1016/j.jor.2022.11.013. PMID: 36471696; PMCID: PMC9718957.
- Piggott RP, Hennessy O, Aresti NA. Distal humerus hemiarthroplasty for trauma: a systematic review of the outcomes and complications. J Shoulder Elbow Surg. 2022 Jul;31(7):1545-1552. doi: 10.1016/j.jse.2022.02.015. Epub 2022 Mar 23. PMID: 35337953.
- Smith GC, Hughes JS. Unreconstructable acute distal humeral fractures and their sequelae treated with distal humeral hemiarthroplasty: a two-year to eleven-year follow-up. J Shoulder Elbow Surg. 2013 Dec;22(12):1710-23. doi: 10.1016/j.jse.2013.06.012. Epub 2013 Sep 20. PMID: 24054974.