More Information
Submitted: May 10, 2023 | Approved: June 07, 2023 | Published: June 08, 2023
How to cite this article: Ruiz PAG, Garrido MR. Dorsal intraspinal B-cell Non-Hodgkin lymphoma in two patients. Arch Clin Exp Orthop. 2023; 7: 015-017.
DOI: 10.29328/journal.aceo.1001015
Copyright Licence: © 2023 Ruiz PAG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Non-Hodking; Lymphoma; Spine; Surgery; Compression
Dorsal intraspinal B-cell Non-Hodgkin lymphoma in two patients
Patricia Alejandra Garrido Ruiz1* and Marta Román Garrido2
1Neurosurgery Department, Salamanca University Hospital, Spain
2Primary Care Department, Salamanca University Hospital, Spain
*Address for Correspondence: Patricia Alejandra Garrido Ruiz, Neurosurgery Department, Salamanca University Hospital, Pº de San Vicente, 182, 37007 Salamanca; Neurosurgery Service: 4th Floor, Block D, Spain, Email: [email protected]
Non-Hodgkin Lymphoma is rarely diagnosed as spinal cord compression syndrome. Caused by an epidural mass, this complication is often encountered in the late stage of the disease. We report two cases presenting symptoms of low thoracic spinal cord compression due to an epidural tumor on the MRI. Possible complications that may occur and how to prevent adverse events during surgery are essential. This case is of special interest for being a low-incidence pathology in a rare location. The case is of high interest because of the importance of resecting the lesion to prevent sequels and the complexity of its management and highlights the importance of considering the diagnosis of this event.
Non-Hodgkin lymphoma is a group of malignant neoplasms originating from the lymphoid tissues, mainly the lymph nodes. It originates from B cell precursors, mature B cells, T cell precursors, and mature T cells. This tumor may result due to chromosomal translocation, various toxins, infections, and chronic inflammation. It comprises various subtypes, each with different clinical features and responses to therapy. It can be mainly divided into two groups, indolent and aggressive, based on the disease’s prognosis. Indolent lymphomas present with waxing and waning lymphadenopathy for many years, whereas aggressive lymphomas have specific B symptoms such as weight loss, night sweats, and fever and can result in death within a few weeks if untreated. Non-Hodgkin lymphoma arises either from B cells, T cells, or natural killer cells due to chromosomal translocation or mutation/deletion. Proto-oncogenes are activated by chromosomal translocation, and tumor suppressor genes are inactivated by chromosomal deletion or mutation. The t (14;18) translocation is the most common chromosomal abnormality in Non-Hodgkin lymphoma. This translocation results in the overexpression of cyclin D1, a cell cycle regulator [1,2]. We present two cases of intramedullary non-Hodgkin lymphoma. The comparison between the two cases is of great interest because it occurs despite being of the same cell lineage with different clinical manifestations and radiological characteristics [3]. Only 0.6% - 6.5% produce spinal neurological complications, the most prone being those with large B cells, affecting only 2/3 of the vertebral level [4-7]. Few patients with intramedullary involvement have been described in the literature, with epidural infiltration being the most common mechanism of spinal neurological complication [8-10].
They are a 77-year-old patient and another 78-year-old. The first presented with right cervicobrachialgia and paresis of the upper limbs. The spinal MRI shows a lesion with the invasion of the C7-T1-T2 vertebral bodies, involvement of the spinal canal, and foraminal stenosis, as well as injury to the pelvis and para-aortic retroperitoneal lymph nodes. The second presented gait instability and paresis in the right leg with allodynia in the left leg and urinary retention. The spinal MRI revealed a well-defined intramedullary lesion suggestive of ependymoma. In both cases, decompressive laminectomies and flavectomy were performed with biopsies, resulting in the first-grade IV large B-cell non-Hodgkin lymphoma, which received radiotherapy and R-CHOP chemotherapy with a significant reduction in tumor mass, and the second high-grade B-cell lymphoma. of malignancy/Intramedullary mantle lymphoma T4-T5. Receiving R-CHOP chemotherapy with a favorable response.
Patient 1
The patient was admitted to the hospital due to cervical-dorsal pain for a year. In the latest weeks, it has worsened, being of great intensity and irradiating mainly towards the right arm. Associated weakness to mobilize both arms, more marked at the distal level. The MRI of the spine shows a lesion invading the C7-D1-D2 vertebral bodies in its anterior region, with involvement of the medullary canal and marked foraminal stenosis at the exit of the C8 roots. A Total Body CT study was carried out where a pelvic lesion was observed, after ruling out the possibility of a biopsy for bone marrow study without significant findings, it was decided to transfer the lesion for a neurosurgical biopsy (Figure 1).
Figure 1: Patient 1: Sagital MRI T2 STIR.
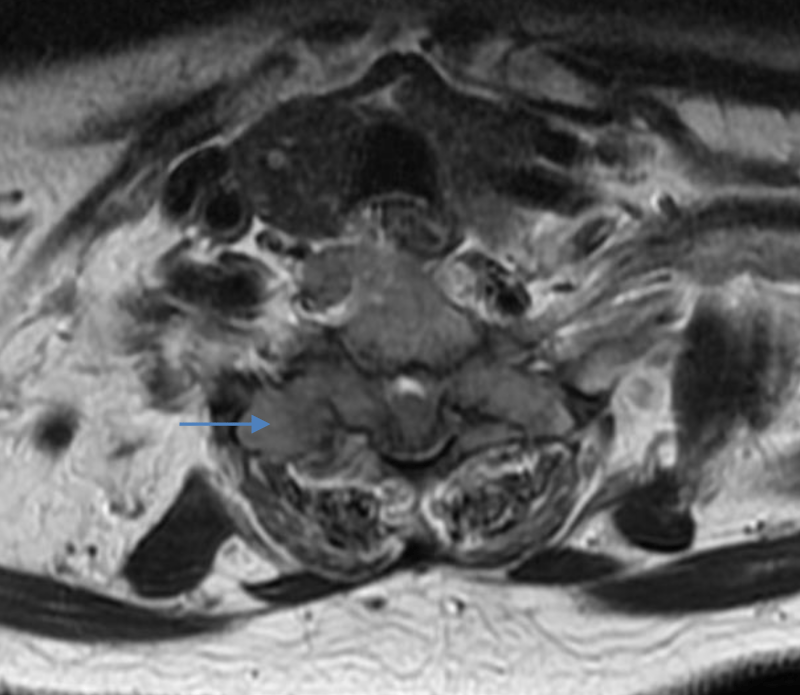
Dorsolumbar MRI
Two bone lesions with a soft tissue mass: one in the bodies in the first and second thoracic vertebrae (blue arrow), showing soft tissue mass centered at C7, D1, D2 and axial T1 showing epidural mass with extension into the posterior elements and lateral masses (Figure 2; blue arrow). Another lesion was found in the pubis and right ischiopubic ramus. Compatible with myeloma or metastasis. Another small lytic lesion on the left scapula, more non-specific, is of doubtful value. Three infrarenal left paraaortic retroperitoneal pathological nodes are related to the same process. Mediastinal nodule, probable ganglion.
Figure 2: Patient 1: Axial MRI T2.
Pulmonary nodules: One of 10 mm in the right lung, it can be a hamartoma, granuloma, or metastasis; and several millimeters in the lingula, probable granulomas and less probable metastasis.
Patient 2
The patient was admitted for scheduled surgery. For months he had presented gait instability with clumsiness in the legs and a sensation of numbness in the distal MMII, diagnosed with polyneuropathy and at the time he was evaluated by Rehabilitation. Progressive symptoms of two weeks of evolution, of leg weakness plus the right with impossibility to walk, in the last week allodynia of the left leg. No bulbar clinic or evident in lower limbs, no back pain. He wasn´t capable to stand up for ten days. Urinary retention since 24h. Partial excision of intramedullary lesion T4-T5 was performed under NFS monitoring (Figure 3).
Figure 3: Patient 2: Sagital MRI STIR.
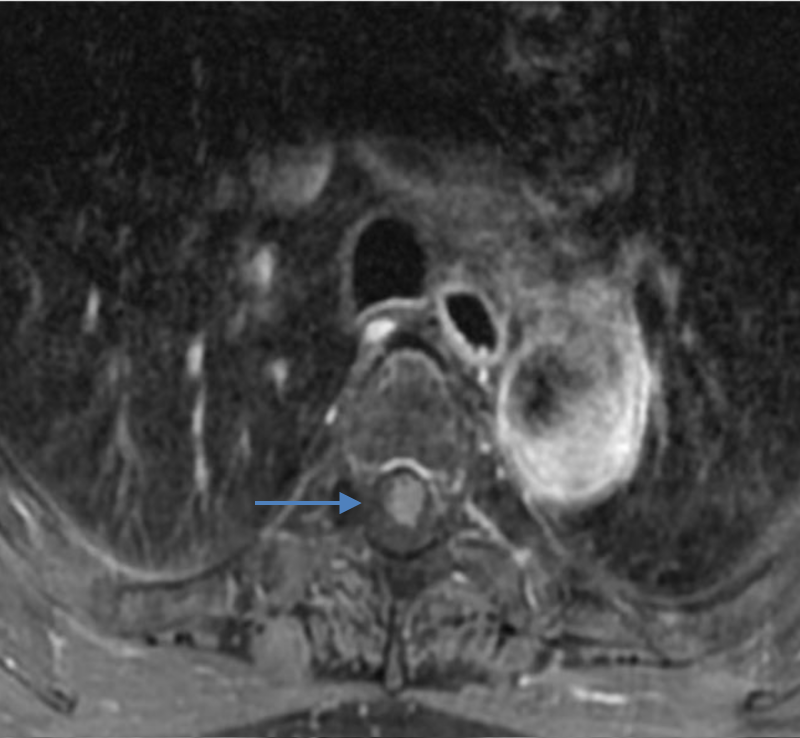
Cervicothoracic MRI
Intramedullary lesion at T4-T5 level (blue arrow), hyperintense with contrast (Figure 4; blue arrow).
Figure 4: Patient 2: Axial MRI T1 with contrast.
Low back pain and radicular pain are frequent complaints, with the most common cause herniated intervertebral disc. Other causes include overgrowth of bone intruding into the spinal canal, spinal stenosis, fracture-dislocation of the spine, infections and neoplasm.
The two patients reported in this paper, who were admitted with neurological signs, suffered from a malignant epidural non-Hodgkin’s lymphoma. Lymphomas are a heterogeneous group of malignancies of B cells or T cells that usually originate in the lymph nodes but may originate in any organ of the body. Extranodal disease is an adverse prognostic factor, particularly the involvement of the Central Nervous System (CNS). Between 5% and 10% of patients with nodal presentation of lymphoma may develop CNS involvement. The intermediate or high histological type of non-Hodgkin’s lymphoma and the presence of an underlying immune deficiency are the most significant risk factors for secondary CNS involvement. CNS presentations may include spinal cord compression, leptomeningeal spread, or intracerebral mass lesions. In addition, other mechanisms of neuropathy should be considered, such as the effects of chemotherapy [11-13].
Spinal cord compression is a rare presentation of non-Hodgkin’s lymphoma, occurring in 0.1% to 3.3% of patients. It is commonly caused by extradural disease, either because of an isolated deposit within the spinal canal or by the extension from an adjacent nodal mass or bone involvement. Less commonly, non-Hodgkin’s lymphoma may arise subdurally or within the spinal cord. Spinal cord compression typically presents with back pain, leg numbness and tingling, radicular pain followed by extremity weakness, paresis and paralysis, but can also be asymptomatic at presentation.
Despite the availability of new techniques for early diagnosis, it can be difficult to differentiate initially serious conditions as an isolated tumoral involvement of the CNS in the absence of widespread disease. Although CNS involvement is most frequently described in intermediate and high-grade non-Hodgkin’s lymphoma, patients with a medical history of low-grade lymphoma can casually develop this kind of involvement. In patients with a history of lymphoma and neurological signs, an MRI of the spine must be performed and is the technique of choice as it is able to identify spinal cord lesions not visible by other radiographic techniques. Although spinal epidural involvement is a rare presentation of non-Hodgkin’s lymphoma, it can be the only symptom of lymphoma and must be considered. Late diagnosis, location of non-Hodgkin’s lymphoma in the cervical and upper thoracic region, rapid progression of neurological deficit and the appearance of paraplegia, and immunosuppression are associated with a worse prognosis. The objective of surgery is decompression and taking biopsies for anatomopathological study [14,15]. Corticosteroids, chemotherapy with a CHOP regimen, local radiotherapy and immunotherapy with Rituximab are used.
Conflict of interest
The authors declare no conflicts of interest and have adhered to the accepted ethical standards by obtaining ethical approval.
- Alexander DD, Mink PJ, Adami HO, Chang ET, Cole P, Mandel JS, Trichopoulos D. The non-Hodgkin lymphomas: a review of the epidemiologic literature. Int J Cancer. 2007;120 Suppl 12:1-39. doi: 10.1002/ijc.22719. PMID: 17405121.
- Solal-Céligny P, Ganem G, Brousse N. Central nervous involvement in Non-Hodgkin's lymphomas. in Non-Hodgkin's lymphomas. eds Solal-Céligny P, Brousse N, Reyes F, Gisselbrecht C, Coiffier B (Editions Frison-Roche, Paris). 1993; 295–300.
- Eeles RA, O'Brien P, Horwich A, Brada M. Non-Hodgkin's lymphoma presenting with extradural spinal cord compression: functional outcome and survival. Br J Cancer. 1991 Jan;63(1):126-9. doi: 10.1038/bjc.1991.25. PMID: 1989650; PMCID: PMC1971629.
- Youmans. Neurological Surgery. 7th Edition. Saunders Company. October 11, 2016.
- Rhoton. Rhoton's Cranial Anatomy and Surgical Approaches. Oxford University Press. Congress of Neurological Surgeons (CNS). 2019.
- M Greenberg. Handbook of Neurosurgery. Thieme, 2019. 9th Edition.
- Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972 Jan;29(1):252-60. doi: 10.1002/1097-0142(197201)29:1<252: aid-cncr2820290138>3.0.co;2-#. PMID: 5007387.
- Mally R, Sharma M, Khan S, Velho V. Primary Lumbo-sacral Spinal Epidural Non-Hodgkin's Lymphoma: A Case Report and Review of Literature. Asian Spine J. 2011 Sep;5(3):192-5. doi: 10.4184/asj.2011.5.3.192. Epub 2011 Aug 12. PMID: 21892393; PMCID: PMC3159069.
- Perry JR, Deodhare SS, Bilbao JM, Murray D, Muller P. The significance of spinal cord compression as the initial manifestation of lymphoma. Neurosurgery. 1993 Feb;32(2):157-62. doi: 10.1227/00006123-199302000-00001. PMID: 8437651.
- Tang Y, Yang X, Xiao J, Liu K, Yan W, Song D, Qu J, Ma J, Wan W. Clinical outcomes of treatment for spinal cord compression due to primary non-Hodgkin lymphoma. Spine J. 2013 Jun;13(6):641-50. doi: 10.1016/j.spinee.2012.11.054. Epub 2013 Jan 19. PMID: 23337542.
- Haemacare-Cancer Registry Based project on Haematologic Malignancies. Background, rationale and aims. March 8, 2010 Eurocare-4.
- Morton LM, Turner JJ, Cerhan JR, Linet MS, Treseler PA, Clarke CA, Jack A, Cozen W, Maynadié M, Spinelli JJ, Costantini AS, Rüdiger T, Scarpa A, Zheng T, Weisenburger DD. Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph). Blood. 2007 Jul 15;110(2):695-708. doi: 10.1182/blood-2006-11-051672. Epub 2007 Mar 27. PMID: 17389762; PMCID: PMC1924473.
- Marcos-Gragera R, Pollán M, Chirlaque MD, Gumà J, Sanchez MJ, Garau I; Non-Hodgkin's Lymphoma Working Group. Attenuation of the epidemic increase in non-Hodgkin's lymphomas in Spain. Ann Oncol. 2010 May;21 Suppl 3:iii90-96. doi: 10.1093/annonc/mdq088. PMID: 20427366.
- Mullins GM, Flynn JP, el-Mahdi AM, McQueen JD, Owens AH Jr. Malignant lymphoma of the spinal epidural space. Ann Intern Med. 1971 Mar;74(3):416-23. doi: 10.7326/0003-4819-74-3-416. PMID: 4928162.
- Wada N, Kohara M, Ikeda J, Hori Y, Fujita S, Okada M, Ogawa H, Sugiyama H, Fukuhara S, Kanamaru A, Hino M, Kanakura Y, Morii E, Aozasa K. Diffuse large B-cell lymphoma in the spinal epidural space: A study of the Osaka Lymphoma Study Group. Pathol Res Pract. 2010 Jul 15;206(7):439-44. doi: 10.1016/j.prp.2010.02.003. Epub 2010 Apr 15. PMID: 20399024.