More Information
Submitted: January 25, 2023 | Approved: February 06, 2023 | Published: February 07, 2023
How to cite this article: Prem A, Anand S. Baxter’s nerve injury: an often overlooked cause of chronic heel pain: a case report. Arch Clin Exp Orthop. 2023; 7: 003-004.
DOI: 10.29328/journal.aceo.1001012
Copyright Licence: © 2023 Prem A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Baxter’s nerve injury: an often overlooked cause of chronic heel pain: a case report
Anand Prem* and Suwarna Anand
Department of Anesthesiology, University of Mississippi Medical Center, Jackson, Mississippi, USA
*Address for Correspondence: Anand Prem, MD, Department of Anesthesiology, University of Mississippi Medical Center, Jackson, Mississippi, USA, Email: [email protected]
Chronic foot and heel pain is a clinical dilemma that Pain Physicians often encounter in their daily practice. In the younger active patients, this is often attributed to plantar fasciitis but other rarer etiologies should also be considered. In patients who present with pain over the medial calcaneus, entrapment neuropathy of the inferior calcaneal nerve, the first branch of the lateral plantar nerve (FBLPN), also known as “Baxter’s nerve” must be considered [1,2]. Initially described in 1984 by Baxter and Thigpen, it is often overlooked as a cause of medial heel pain, particularly in athletes, where it may coexist with plantar fasciitis [3]. The nerve has a tortuous course in the foot and can be entrapped as it passes through the fascia of the abductor hallucis, travels in close proximity to a plantar spur or the medial calcaneal tuberosity, or gets enmeshed in scar tissue from prior surgery [1,3].
Working knowledge of the anatomy of the foot, astute physical examination skills, a high index of suspicion, and the use of appropriate diagnostic/therapeutic local anesthetic blocks are key factors that lead to a timely diagnosis and optimal management of these patients, enabling a prompt return to an active lifestyle.
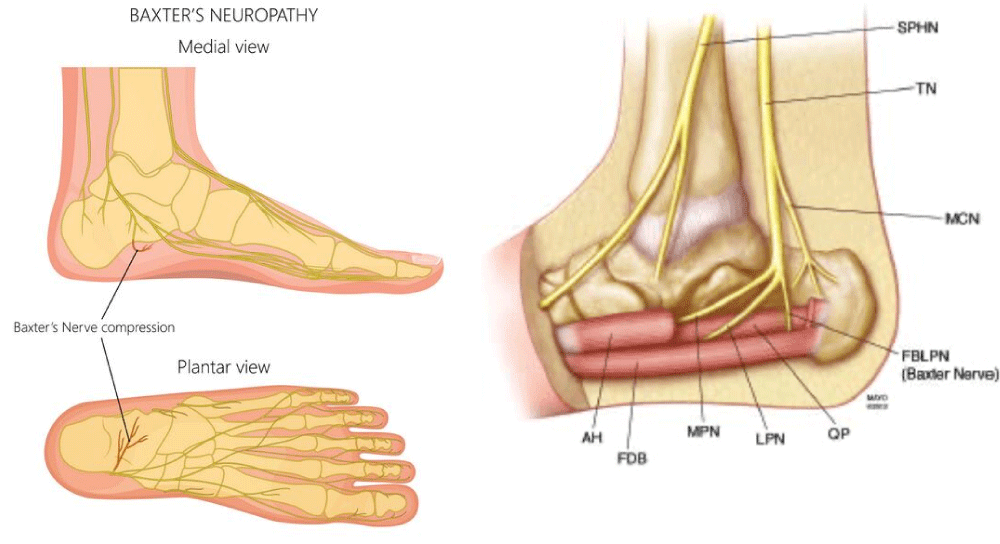
This case report details a case of complete resolution of pain in a patient with long-standing history of intractable heel pain following a block of the Baxter’s nerve with local anesthetic and steroids Figure 1.
Figure 1: Complete resolution of pain in a patient with long-standing history of intractable heel pain. SPHN: Saphenous Nerve; TN: Tibial Nerve; MCN: Medial Calcaneal Nerve; FBPLN: First Branch of Lateral Plantar Nerve (Baxter’s nerve); QP: Quadratus Plantae; LPN: Lateral Plantar Nerve; MPN: Medial Plantar Nerve; FDB: Flexor Digitorum Brevis; AH: Abductor Hallucis.
• This is a medically challenging case and IRB approval is not required in the absence of PHI per UMMC policy.
• Patient informed consent was obtained for the submission of this case report.
• All patient-protected health information has been de-identified.
A 22-year-old Caucasian male triathlete presented to our clinic with chronic medial Left heel /foot pain for the past nine months. He described the pain as intermittent, dull at times but sharp and excruciating during exacerbations brought on by running. 6 months ago, he had surgery to remove a heel spur with about 50% improvement in pain for about 2 months. Thereafter he had a recurrence of pain in the proximal heel, occasionally radiating laterally over the plantar aspect of the foot, with tingling and numbness, worsening as the day progressed. He denied significant pain on waking.
In the course of his work up to diagnose this pain, he had X-rays of his Left foot and ankle which did not reveal any fracture. Failed medical therapy included rest, activity modification, PT, Meloxicam, Pregabalin and Gabapentin. A presumptive diagnosis of plantar fasciitis was made and the patient was prescribed Physical Therapy with minimal improvement in pain. An ultrasound guided local anesthetic + steroid injection of the plantar fascia gave about 30% temporary relief of his distal foot pain but heel pain persisted.
Subsequent Ankle MRI showed no evidence of Achilles tendinopathy, mild thickening and inflammation of the proximal fascia and fatty infiltration, and mild atrophy of the abductor digiti minimi muscle (ADMM). The exam was positive for maximal tenderness just distal to the medial calcaneal tuberosity. Phalen’s test (passive inversion and plantar flexion of the foot) was positive with diminished sensation over the lateral plantar aspect of the foot.
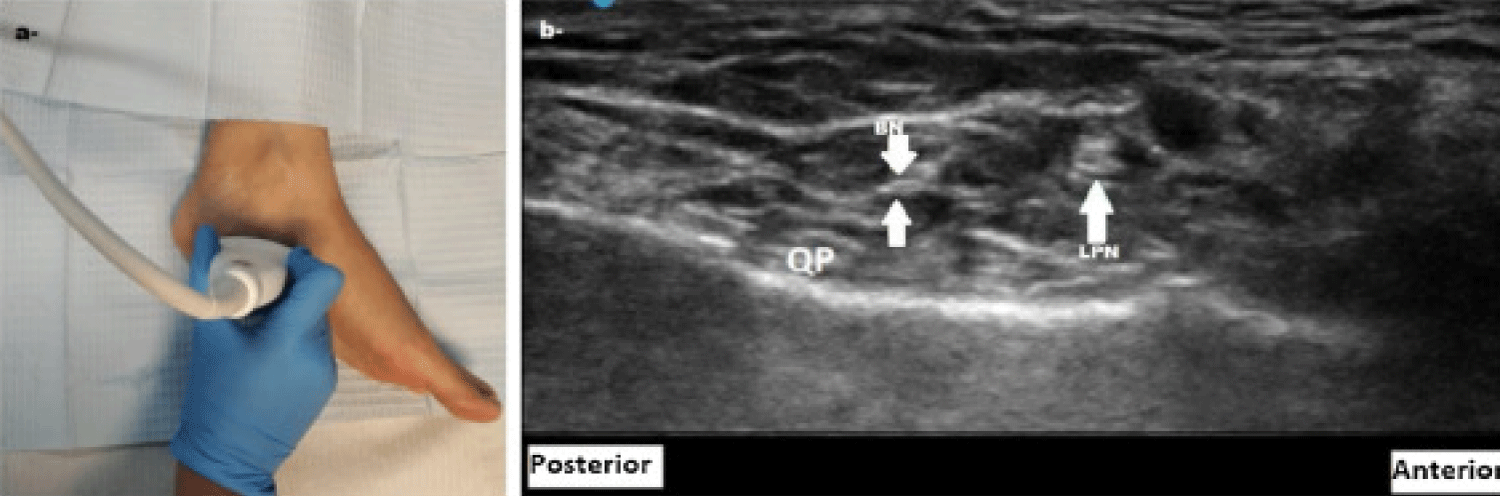
The patient was then scheduled for an ultrasound-guided diagnostic “Baxter nerve” block. The block was accomplished uneventfully using a 22 G 2-inch echogenic Stimuplex needle using an out-of-plane, posterior to anterior approach with 2 ml of 0.5% Bupivacaine and 40 mg Depomedrol, medial and proximal to the calcaneal origin of the plantar fascia. The injectate was seen to spread in the fascial plane over the Quadratus Plantae (QP) muscle. The patient tolerated the procedure well with excellent pain relief. At the time of discharge, his Pain Score was down to 0/10 from a Pre-procedure Pain Score of 7/10.
Since the nerve block, he has been seen on 2 follow-up visits over the past 8 months and continues to report an almost complete resolution of pain. Over the past 4 months, he has resumed running with no limitations Figure 2.
Figure 2: Over the past 4 months, he has resumed running with no limitations. BN: Baxter Nerve; LPN: Lateral Plantar Nerve; QP: Quadratus Plantae.
Baxter’s nerve entrapment can often masquerade as plantar fasciitis, particularly when encountered in active younger patients [2-4]. This first branch of the lateral plantar nerve may become entrapped between the ADMM and medial calcaneal tuberosity or a heel spur and cause neuropathic pain symptoms located on the medial arch of the foot [1]. It often presents with sharp, burning pain, associated with numbness and tingling around the medial heel, radiating to the lateral foot mimicking the typical course of the nerve. Baxter’s nerve entrapment can also occur after repetitive microtrauma of the heel or from entrapment within scar tissue from prior surgery, as seen in this case [3-5]. The condition is not gender or age specific and is worsened by passive eversion or abduction of the foot. While pain in plantar fasciitis is worse in the morning after a period of rest or inactivity, Baxter nerve entrapment pain worsens with weight-bearing activity as the day progresses. It can account for up to 20% of the cases of chronic heel pain [1,3,4]. Radiographic imaging studies are of limited diagnostic value in detecting any nerve entrapment, though occasionally atrophy in the abductor digiti minimi muscle or surrounding scar tissue may be picked up by MRI. High-resolution ultrasound is being increasingly used to identify nerve entrapment [5].
Surgical decompression of the nerve may be an option for intractable cases confirmed by diagnostic blocks that do not respond to conservative therapy. Rehabilitation is key to maintaining therapeutic benefit [2,5,6].
With the opioid crises front and center, it is all the more important to make the correct diagnosis clinically to formulate an effective treatment plan. A delay in diagnosis can result in prolonged periods of ineffective treatment, frustration, and persistent pain with significant impairment of physical activity, especially in the younger population. A thorough knowledge of the anatomy of the foot and its innervation, and good physical examination skills supported by appropriate imaging and diagnostic/therapeutic blocks can put the patient on the path to recovery.
- Moroni S, Zwierzina M, Starke V, Moriggl B, Montesi F, Konschake M. Clinical-anatomic mapping of the tarsal tunnel with regard to Baxter's neuropathy in recalcitrant heel pain syndrome: part I. Surg Radiol Anat. 2019 Jan;41(1):29-41. doi: 10.1007/s00276-018-2124-z. Epub 2018 Oct 27. PMID: 30368565; PMCID: PMC6514163.
- Presley JC, Maida E, Pawlina W, Murthy N, Ryssman DB, Smith J. Sonographic visualization of the first branch of the lateral plantar nerve (baxter nerve): technique and validation using perineural injections in a cadaveric model. J Ultrasound Med. 2013 Sep;32(9):1643-52. doi: 10.7863/ultra.32.9.1643. PMID: 23980227.
- Baxter DE. Release of the nerve to the abductor digiti minimi. In: Kitaoka HB, ed. Master techniques in orthopedic surgery of the foot and ankle. Philadelphia, PA: Lippincott Williams and Wilkins; 2002: 359.
- Beltran LS, Bencardino J, Ghazikhanian V, Beltran J. Entrapment neuropathies III: lower limb. Semin Musculoskelet Radiol. 2010 Nov;14(5):501-11. doi: 10.1055/s-0030-1268070. Epub 2010 Nov 11. PMID: 21072728.
- Allam AE, Chang KV. Plantar Heel Pain. 2022 Sep 5. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan. PMID: 29763043.
- Lareau CR, Sawyer GA, Wang JH, DiGiovanni CW. Plantar and medial heel pain: diagnosis and management. J Am Acad Orthop Surg. 2014 Jun;22(6):372-80. doi: 10.5435/JAAOS-22-06-372. PMID: 24860133.