More Information
Submitted: January 17, 2023 | Approved: January 24, 2023 | Published: January 25, 2023
How to cite this article: RodríguezAngelov M, Tivcheva Y, Krastev D, Krastev N. Anterolateral ligament: A case report. Arch Clin Exp Orthop. 2023; 7: 001-002.
DOI: 10.29328/journal.aceo.1001011
Copyright Licence: © 2023 Angelov M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Anterolateral ligament: A case report
Mihail Angelov1* , Yoanna Tivcheva1, Dimo Krastev2,3 and Nikolai Krastev1
, Yoanna Tivcheva1, Dimo Krastev2,3 and Nikolai Krastev1
1Department of Anatomy, Histology and Embryology, Medical University of Sofia, 2 Zdrave Street, 1431 Sofia, Bulgaria
2Medical College “Jordanka Filaretova”, Medical University of Sofia, 3 Jordanka Filaretova Street, 1606 Sofia, Bulgaria
3Faculty of Public Health, Health Care and Sport, South-West University “Neofit Rilski”, 66 Ivan Mihailov Street, 2700 Blagoevgrad, Bulgaria
*Address for Correspondence: Mihail Angelov, Department of Anatomy, Histology and Embryology, Medical University of Sofia, 2 Zdrave Street, 1431 Sofia, Bulgaria, Email: [email protected]
The Anterolateral Ligament (ALL) [1,2] is a ligamentous structure of the knee whose definition as a ligament has been disputed in the past, however in the last decade more and more anatomical studies have concluded that its definition as a separate ligament is the most accurate. In this case report we present our findings from the dissection of a formalinized cadaver which we find are consistent with the anatomical characteristics of the anterolateral ligament and with that we aim to further its morphological definition.
The ALL is an extracapsular ligament located at the anterolateral aspect of the knee and anteriorly to the lateral collateral ligament that stabilizes the knee joint during internal rotation [3]. Its point of origin is the lateral epicondyle of the femur and it attaches distally to the anterolateral aspect of the tibia, between the tubercle of Gerdy and the head of the fibula. The original report on the existence of this ligamentous structure was by the french surgeon Paul Segond in 1879. He described the structure as a fibrous thickening of the capsular wall and related it to the “Segond fracture” [4]. The Segond fracture is an avulsion fracture of the lateral aspect of the tibial plateau which is considered pathognomonic of a rupture of the anterior cruciate ligament [1,5]. More recent cadaveric studies have discovered the ligament as well and defined it as a ligamentous structure on the anterolateral aspect of the knee [2,6].
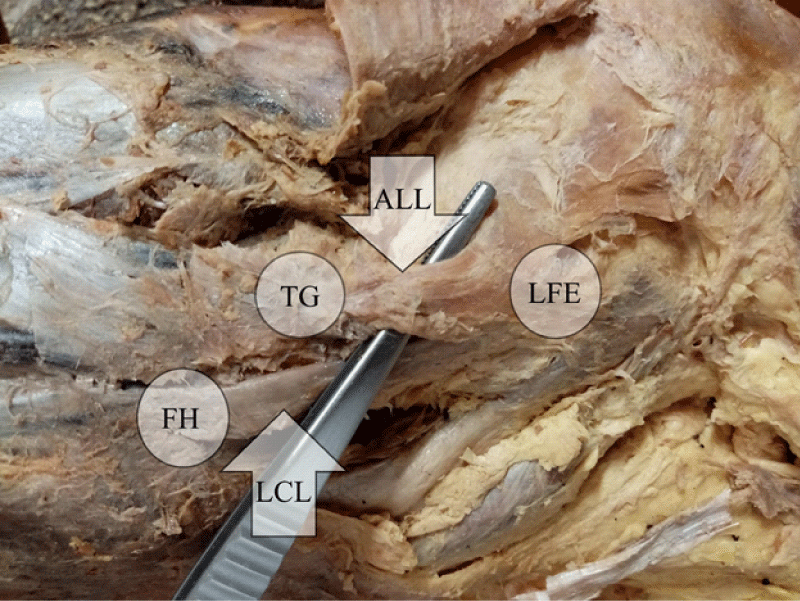
During a routine dissection of a formalinized female Caucasian cadaver at the department of Anatomy, Histology and Embryology at the Medical University of Sofia, we discovered an extracapsular band of dense connective tissue, with firmness and lack of elasticity that was akin to that of a ligamentous structure, on the right knee beneath the iliotibial tract. The structure was 43 mm in length and 3 mm in thickness with a point of origin being the lateral femoral epicondyle, superiorly and posteriorly in relation to the origin of the lateral collateral ligament of the knee and its point of attachment being between the tubercle of Gerdy and the head of the fibula. Upon close examination we discovered insertions in the lateral meniscus of the knee and the joint capsule (Figure 1).
Figure 1: ALL: Anterolateral Ligament; LCL: Lateral Collateral Ligament; LFE: Left Femoral Epicondyle; TG: Tubercle of Gerdy; FH: Fibular Head
Our findings are consistent with the modern definition of the ALL. Studies have shown that the anterolateral ligament has an overall prevalence of 45% to 97% [2,7]. There still are however some aspects of the ligament which are yet to be elucidated. Recent studies [8] into the histological architecture of the anterolateral ligament have shown much closer histological similarities to the Anterior Cruciate Ligament (ACL) than previously believed. The orientation of the collagen fibers, the cellularity and presence of nerve fibers are all characteristics that show closer similarity to the ACL than with the structure of the joint capsule. The need for ALL reconstruction with the aim being improving the rotational stability of the knee is still a point of contention between orthopedic surgeons because of the inconsistent data on the ALL [9] even though data so far has shown improved rotational stability and reduced anterior translation of the tibia in patients who have had a combined ALL and ACL reconstruction in comparison to just an ACL reconstruction [10]. Furthermore, there still isn’t a consensus on which surgical technique yields the best results if the surgeon opts for reconstructing the ALL. One study in particular, carried out by Iderhaug, et al. [11] compared the results of isolated ACL reconstruction and combined ALL and ACL reconstruction using a gracilis tendon autograft, modified MacIntosh ALL tenodesis in combination with ACL reconstruction, modified Lemaire tenodesis in combination with ACL reconstruction and a further modified Lemaire tenodesis with ACL reconstruction. The results from this study demonstrated that the modified MacIntosh ALL tenodesis and the modified Lemaire tenodesis in combination with ACL reconstruction showed much better rotational stability and reduced anterior tibial translation when compared to isolated ACL reconstruction, however the results did not support ALL reconstruction in combination with ACL reconstruction due to the fact that this procedure failed to restore the native kinematics of the joint.
Further anatomical and histological studies are needed to completely elucidate the role of the ALL in the biomechanics of the knee, its possible role in operative stabilization of the joint after ACL ruptures and the role of the ligament in proprioception. To that end more cadaveric studies are needed to ascertain the definitive morphological characteristics, point of origin and site of insertion of the ligament [9]. Furthermore the exact effect that the ALL has on the biomechanics of the joint is still not definitively determined due to inconsistencies in the results during tests [6,12].
Author contributions
MA and JT performed the dissection, DK and NK were consultants on how the dissection should be performed and the clinical relevance of the case, MA wrote the case report.
- Segond P. Clinical and experimental research on sprained knee blood effusions. Medical Progress. Paris. 1879; 1‐85.
- Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013 Oct;223(4):321-8. doi: 10.1111/joa.12087. Epub 2013 Aug 1. PMID: 23906341; PMCID: PMC3791125.
- Woods GW, Stanley RF, Tullos HS. Lateral capsular sign: x-ray clue to a significant knee instability. Am J Sports Med. 1979 Jan-Feb;7(1):27-33. doi: 10.1177/036354657900700107. PMID: 420385.
- Hess T, Rupp S, Hopf T, Gleitz M, Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res. 1994 Jun;(303):193-7. PMID: 8194233.
- Hess T, Rupp S, Hopf T, Gleitz M, Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res. 1994 Jun;(303):193-7. PMID: 8194233.
- Grimshaw P, Jones C, Lock M, Longbottom M. The Biomechanics of the Anterolateral Ligament. Recent Advances in Biomechanics. 2020. doi: 10.5772/intechopen.92055.
- Runer A, Birkmaier S, Pamminger M, Reider S, Herbst E, Künzel KH, Brenner E, Fink C. The anterolateral ligament of the knee: A dissection study. Knee. 2016 Jan;23(1):8-12. doi: 10.1016/j.knee.2015.09.014. Epub 2015 Dec 31. PMID: 26749203.
- Sabatini L, Risitano S, Atzori F, Volante M, Aprato A, Indelli PF, Massè A. Histological analysis of the anterolateral ligament of the knee. J Orthop. 2019 Apr 8;16(5):368-372. doi: 10.1016/j.jor.2019.03.019. PMID: 31011250; PMCID: PMC6463743.
- Ahn JH, Patel NA, Lin CC, Lee TQ. The anterolateral ligament of the knee joint: a review of the anatomy, biomechanics, and anterolateral ligament surgery. Knee Surg Relat Res. 2019 Nov 28;31(1):12. doi: 10.1186/s43019-019-0012-4. PMID: 32660576; PMCID: PMC7219606.
- Ibrahim SA, Shohdy EM, Marwan Y, Ramadan SA, Almisfer AK, Mohammad MW, Abdulsattar WS, Khirat S. Anatomic Reconstruction of the Anterior Cruciate Ligament of the Knee With or Without Reconstruction of the Anterolateral Ligament: A Randomized Clinical Trial. Am J Sports Med. 2017 Jun;45(7):1558-1566. doi: 10.1177/0363546517691517. Epub 2017 Feb 1. PMID: 28293966.
- Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical Comparison of Anterolateral Procedures Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017 Feb;45(2):347-354. doi: 10.1177/0363546516681555. Epub 2016 Dec 27. PMID: 28027653.
- Lee JK, Seo YJ, Jeong SY, Yang JH. Biomechanical function of the anterolateral ligament of the knee: a systematic review. Knee Surg Relat Res. 2020 Jan 1;32(1):6. doi: 10.1186/s43019-019-0021-3. PMID: 32660580; PMCID: PMC7219217.