More Information
Submitted: 17 April 2020 | Approved: 28 May 2020 | Published: 29 May 2020
How to cite this article: Cirotteau Y. Preventive treatment in an osteoporotic femoral upper metaphysis-A clinical case: Me Louise V.... Arch Clin Exp Orthop. 2020; 4: 009-012.
DOI: 10.29328/journal.aceo.1001008
Copyright Licence: © 2020 Cirotteau Y. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Preventive treatment in an osteoporotic femoral upper metaphysis-A clinical case: Me Louise V…
Yves Cirotteau*
191 University road 75007, Paris, France
*Address for Correspondence: Yves Cirotteau, 191 University road 75007 Paris, France, Tel: 33+621888265; Email: [email protected]
In 1992, a patient, born July 10, 1910, aged 82, with major osteoporosis [1-3], was operated on her left hip. The surgeon performs a biomaterial transplant using natural coral [4]. Follow-up is two years. She died in 1994 of acute respiratory failure. Three bone graft osteodensitometry [5] shows a regular increase in mineralization; however, on the opposite side, bone mineralization decreases. The anatomical part is examined using x-rays, scanners, photographs, histology [6]. The article reports the findings of this study. It is noted a partial resorption of the biomaterial essentially at the periphery of the graft as well as the different local connections of the preexisting bone with the newly formed bone from the grafted area. The severity of fractures of the femoral neck is no longer to be demonstrated [7]. Multiple therapeutic trials have demonstrated their effectiveness [8,9]. Twenty two patients were transplanted. There was no failure. All died without fracturing their grafted hips.
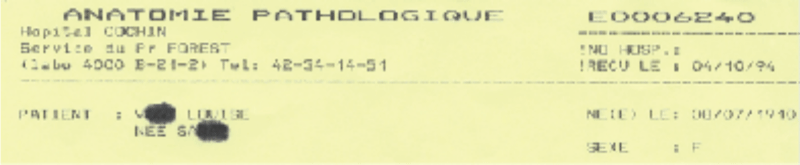
She is a person born on October 2, 1992, living in EPAD. She underwent a hysterectomy with oophorectomy at the age of 29! She has been treated for more than thirty years with 15 mg of cortisone, due to severe asthma. She walks with difficulty, helped by physiotherapists. She cannot go up or down stairs due to her respiratory condition. There is no pain in the hips. She accepts the transplant. This was done on October 2, 1992. Three bone densitometry tests were performed three months, thirteen months and twenty months after the transplant. When the patient died, two years after the transplant, a histological examination of the transplanted hip was entrusted to Professor Maurice-Michel Forest, anatomo-pathologist at Cochin Hospital.
Intervention: Under epidural anesthesia, short external incision centered on the greater trochanter. Several biopsies only bring blood. The surgeon fills the gap with three bottles of natural coral granules [10]. Three-point closure. The patient was put in the chair the next day with immediate support.
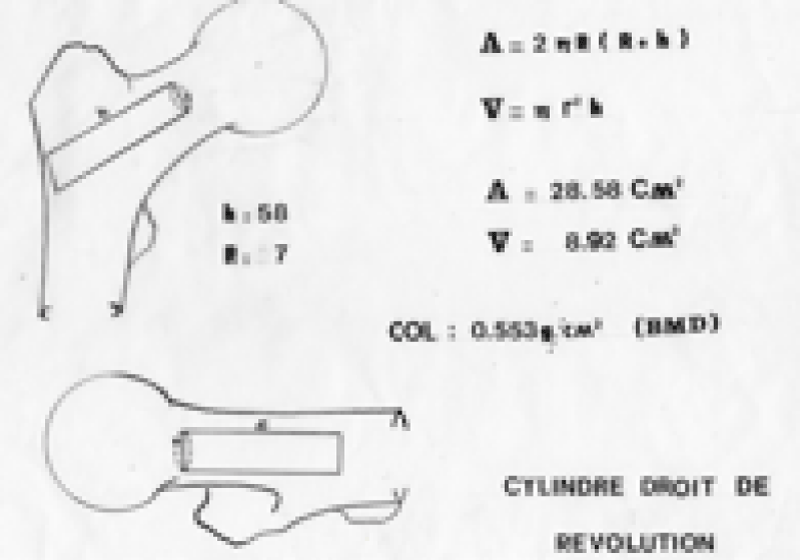
GRAFT TECHNIC: Ccalculation of the Surface (A) and volume (V) of the graft (Figure 1).
Figure 1: Right cylinder of revolution.
GRAFT: Three sachets of three grams in natural coral granules [11-18], were filled in the femoral upper metaphysis.
Operating suites
They were simple. Support was given the next day and the march resumed with the help of physiotherapists. As soon as the skin healed, there were thirty minutes of daily balneotherapy.
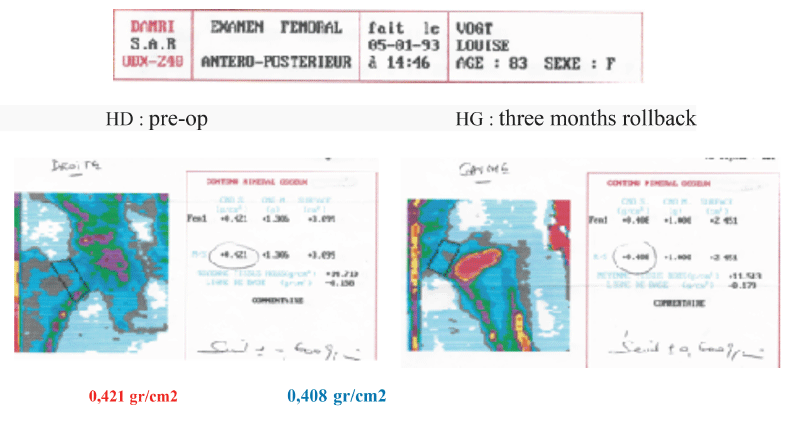
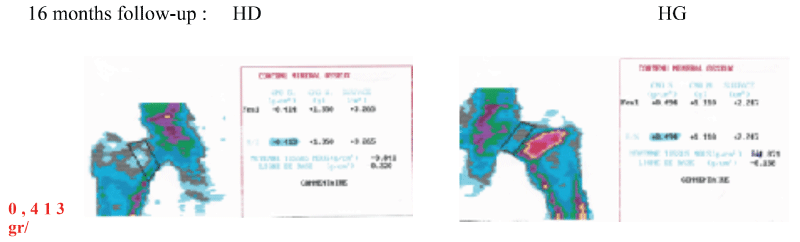
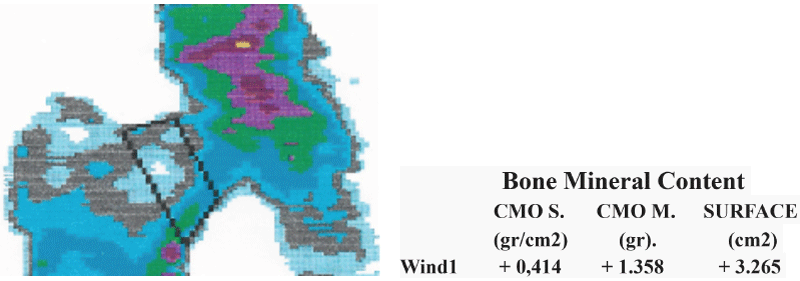
Bone densitometry
Three bone densitometries were performed by the same operator, with the same equipment, under the same conditions.
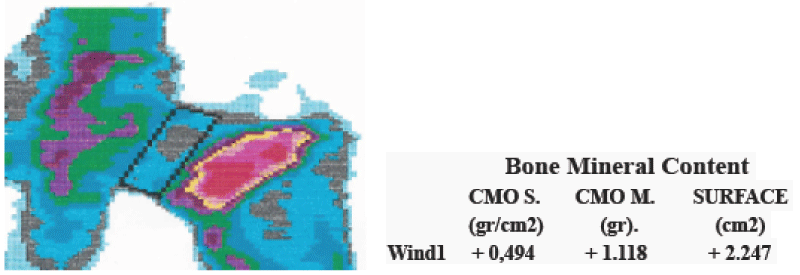
The BMD (Bone Mineral Density) is stable on the right hip and there is a statistically significant gain of 88 mg/c2 in the grafted hip.
Choice of explored areaIn order to eliminate any measurement error of the Bone Mineral Content linked to the presence of the natural coral graft, the explored area was chosen at the head-neck junction, outside the grafted area as can be seen in this image. The increase in D.M.O is only linked to the transformation of the mineral graft content into new-formed bone.
For the same reasons, the area explored is located exactly at the head-neck junction in order to compare what is comparable - according to the Cartesian scientific method. This examination was not easy because the patient is 84 years old. The technical prowess of this examination is to be attributed to Dr J. Jabre.
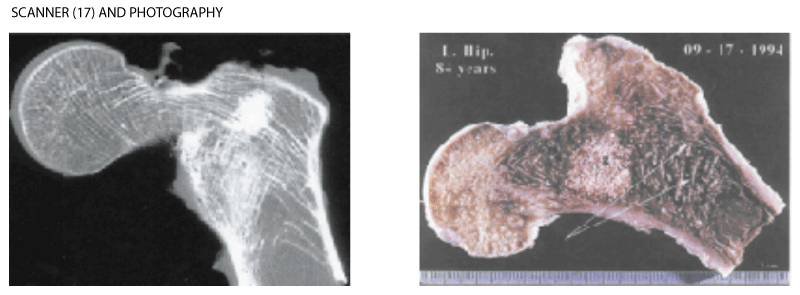
Histological examination
The Morphological modifications of the upper femoral metaphysis are conform to those described previously in other works [3].
Right femoral head: The histological study carried out at the level of the cervical site confirms the clinical notions: there is a major osteoporosis leading to vast ranges of rarefaction filled by an adipose or hematopoietic marrow without cytological lesions. At the level of the cancellous lamellae there are numerous microfractures and multiple organized microcals.
Left femoral head (coral transplant 1992): The center of the coral filling includes a connective tissue surrounding the granules. There are some lymphoplasmocytic infiltrates and rare giant resorptive cells. There is no osteogenesis at this level and the granules are detectable.
At the periphery, there is a complete or incomplete osteogenesis around the granules, the degree of calcification of which is variable. Often there is only immature bone. Contacts with the neighboring cancellous are very variable: simple backing, continuity of neoformed osteogenesis with the peripheral lamellae at some points or interposition of fibrous tissue. Osteoporosis on the left is just as important with the presence of microcals.
Preventive treatment in a person with severe osteoporosis is justified in more ways than one:
A: We know all the multiple risk factors: Globally, the risk factors for developing osteoporosis are multiple: high age, ethnicity, female gender, family history of femoral neck fracture, excessive consumption of salt, alcohol, coffee and tobacco, low body mass index, certain calcium, protein, and vitamin D deficiencies, physical inactivity, immobilization, weightlessness, castration, sex hormone deficiency, certain therapies (corticosteroids, Hypo-thyroid).
B: Bone Mineral loss can be measured by densitometry. The lower it is, the more severe the fracture and the more difficult it’s surgical treatment.
C: We know the fracture threshold (0.600 gr/cm2), below which there is a high risk of fracture due to a simple fall in his or her height.
D: We can predict the age when we reach this threshold.
E: When your femoral neck is broken, there is an 80% risk of having it happen within a year of a contralateral fracture.
F: The older the person, the greater the risk of anesthetics.
G: We know the serious sequelae after surgical treatment of cervical fractures in the elderly. In addition to the mechanical consequences that are all the more important since the fracture is complex, the psychological repercussions can be a real handicap for reintegration into social life.
H: When a hip is fractured, it is easy to preventively treat the other side at the same time. Knowing these parameters, it makes sense to offer preventive treatment or just think of it.
First conclusion: We note that even microfractures of the cancellous lamellae may heal whatever the âge.
Second conclusion: We note that the natural coral graft in contact at the periphery with what remains of intra-metaphyseal spongy bone can form osteoid tissue whose degree of calcification is variable. We can logically deduce that the physiological metabolic functioning of a long bone continues throughout life. In this case, the B.M.D. increased by 88 mg / cm2 in 16 months.
Third conclusion: Natural coral behaves as in a B.M.U. After the phase of demineralization by osteoclasts, there follows a phase of re-mineralization by osteoblasts. Since this process is physiological, there is no risk of failure. The process is 100% safe.
Fourth conclusion: Since natural coral is purely mineral (98% calcium), there is no risk of rejection of the immunological order. The process is 100% safe. The purification process developed by Professor Yann Le Petitcorps’ team eliminates all foreign proteins to the core. There is no risk of rejection of this fact. The process is 100% safe [19].
Five conclusion: The newly formed bone is distributed along the lines of force exerted on the cervico-metaphyseal overhang as shown by the scanner. The osteoid tissue, as well as the newly formed bone, is distributed at a distance from the graft as shown by the various osteo-densitometry.
Fifth conclusion: In the beginning of our experiment, we did not knew the role of bone marrow in the metaplasia of cancellous and cortical bone. We were grafting a coral skeleton without any living cells. In this situation, it’s properties were very different from those of an autologous cancellous living bone graftning. The living cells enhance the metaplastic process. Despite this lack of living cells, despite the âge, the graft started to work.
The surgeon’s honor is to be aware of new tretment, the surgeon’s honor is to keep abreast of the latest treatment novelties, he must ensure that these novelties are true and healthy, that they are not fake-news. The surgeon’s honor must be sure that the new treatment that the new treatment does not produce any side effects or secondary complications. The treatment must be easy to use and fully effective. The biomaterial ( natural coral ) has all its qualities. What are they waiting for ? « I have a dream ! » Curiously it comes to my mind a very unhealthy thought. I will die before I see the dawn. Twenty-two affected patients were transplanted. There were no hip fractures grafted during the time of clinical observation. Two other patients died unrelated to their bone pathology. Surgeons have full cart
The surgeons have their hands full of aces. Patients hope and expect a cure for their problems. What are surgeons waiting for to distribute the winning cards?
- Cirotteau Y. Upper femoral metaphysis morphological modifications of a human struck down by osteoporotic disease. C.R. Acad. Sci. Paris, Sciences de la vie / Life Sciences. 1999; 322: 401-411.
- Cirotteau Y. Morphological modifications of a human bone diaphysis. Theoretical therapeutic deductions. The Surgical Letter. Special issue S.O.F.C.O.T. 1994. N° 128.
- Bone Tissue. L. Theo, J. Vidal, J. Dossa. Coll. Biologie de l’appareil Locomoteur, Sauramps medical. 1989; 67-74.
- Cirotteau Y. Behavior of natural coral in a human osteoporotic bone. Eur J Orthop Surg Traumatol. 2001; 11: 149-160.
- Osteodensitometries are made by biphotonic absorptiometry with no danger of radiation by the use of micro-doses. Hologic QDRqooo/W (S/N 851). They are performed by C. Bergot MD. Service de radiologie, Pr M. Laval-Jeantet MD, Head of service, H6pital Saint Louis, Paris.
- Histological technic: After formalin fixation followed by decalcification, specimens taken from various areas were embedded in paraffin and multiple histologic step sections were prepared which were stained with hematoxylin-eosin-saffron and studied with polarized light. Samples were treated macroscopilcally and microscopically.
- Pison G. The aging of the population. Cahiers d'Anthropologie et Biométrie Humaine.1995; XIII, n°1-2: 39-48.
- Cornell CN. Management of fractures in patients with osteoporosis. Orthop Clinical North Am. 1990; 21: 125-141.
- Barrios C. Healing Complications after internal fixation of trochanteric hip fractures: The prognostic value of osteoporosis. J Orthop Trauma. 1993; 7: 438-442. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8229380
- Patat JL. Study of bone habitation of porous material and irregular surface, Doctoral Thesis in Medicine. University of Paris V. 1976.
- Viateau V, Guillemin G, Bousson B, Oudina K, Hannouche D, et al. Long-bone Critical-Size Defects Treated With Tissue-Engineered Grafts: A Study on Sheep. J Orthop Res. 2007; 25: 741-749. PubMed: https://pubmed.ncbi.nlm.nih.gov/17318898/
- Kehr PH, Graftiaux AG, Gosset F, Bencheikh K. Use of coral in cervical intersomatic grafting. Biomineralization 93, 7th intern. Symp on Biominer Monaco. 1993; N*I4: 123-128.
- Guillemin G, Fournie J, Patat JL, Chetail M. Fate of a Fragment of Madrepore Coral Skeleton Implanted in the Diaphysis of Long Bones in Dogs. CR Acad Sci Paris. 1981; 293: 371-376. PubMed: https://pubmed.ncbi.nlm.nih.gov/6119143/
- Guillemin G, Meunier A, Dallant P, Christel P, Pouliquen JC, et al. Comparison of coral resorption and bone apposition with two natural corals of different porosities. J Biomed Mater Res. 1989; 23: 765-779. https://www.ncbi.nlm.nih.gov/pubmed/2738087
- Ouhayoun P, Issahakian S, Patat JL, Shabana AHM, Guillemin G. Histological evaluation of natural coral skeleton as a grafting material in miniature swine mandible. J Materials Science. 1992; 3: 222-228
- Marchac D, Sandor G. Experience with the use of coral granules in the craniofacial skeleton. J Craniofacial Surgery. 1994; 5: 213-217.
- Scanner technic: All soft issues are removed; The simples are embedded in a wet sheet and put under the machine (80 KV- 100 mA) in a frontal plane. 20 cuts, every 1,5 mm, are made from the anterior (1) to the posterior ( 20) side of both samples.
- Laboratoire Carat: state of knowledge on coral: Morphology, Porosity, Crystal structure, Chemical composition, Mechanical resistance, New purification process. CNRS of Bordeaux. 1999-2005.
- Le Petitcorps Yann, Jean-Christophe Fricain, Vincent Souillac, Mathieu Augustin, Purification of the coral and modification of the product, Lab-Adisseo